Enlarged Prostate
Prostatitis
What is prostatitis?
Prostatitis is inflammation of the prostate gland and sometimes the area around it. It is not cancer.
Only people assigned male at birth have a prostate gland. It sits in front of the rectum and below the bladder. The gland wraps around the urethra, the tube that carries urine out of the body. The prostate makes the fluid part of semen.
Types of prostatitis
- Chronic prostatitis (chronic pelvic pain syndrome) This is the most common type of prostatitis. Symptoms may get better and then come back without warning. Healthcare providers do not know why this happens. There is no cure, but you can manage symptoms.
- Acute bacterial prostatitis. This is the least common type of prostatitis. It happens at any age. It often starts suddenly and causes severe symptoms. It’s important to get treatment right away. You may find it hard and very painful to pee (urinate). Other symptoms include fever, chills, low back pain, pain in the genital area, frequent peeing, a burning feeling when peeing, or urinary urgency at night. You may also have aches and pains all over your body.
- Chronic bacterial prostatitis. This type is fairly uncommon. It is an infection that comes back again and again, and it is hard to treat. Symptoms are like a mild form of acute bacterial prostatitis. But they last longer. Often you have no fever.
- Asymptomatic inflammatory prostatitis. This is prostatitis with no symptoms. Your healthcare provider often diagnoses it during an exam or test, such as a prostate biopsy, for another health problem. They may diagnose it if you have infection-fighting cells in your prostate fluid or semen.
What causes prostatitis?
Prostatitis is most often caused by bacteria. They spread from the rectum or from infected urine.
You can't get prostatitis from another person. It is not a sexually transmitted infection (STI). But it can result from several STIs.
Who is at risk for prostatitis?
You can get prostatitis at any age. But some things raise your risk:
- Recent bladder or urinary tract infection, or other infection in the body
- Injury to the area between the scrotum and the anus
- Abnormal urinary tract anatomy
- Enlarged prostate
- Recent test where a catheter or scope was put into the urethra
What are the symptoms of prostatitis?
These are the most common symptoms of prostatitis:
- Need to pee often
- Burning or stinging feeling when peeing
- Pain when peeing
- Less urine when you pee
- Rectal pain or pressure
- Fever and chills (often only with an acute infection)
- Pain in your low back or pelvis
- Discharge through the urethra during bowel movements
- Erectile dysfunction or loss of sex drive
- Throbbing sensations in the rectal or genital area
The symptoms of prostatitis may look like other health conditions or problems. Always see your healthcare provider for a diagnosis.
How is prostatitis diagnosed?
Your healthcare provider will review your past health and sexual history. They will also do a physical exam. Other tests may include:
- Urine culture. This test collects prostatic fluid and urine. They are checked for white blood cells and bacteria.
- Digital rectal exam (DRE). In this test, the healthcare provider puts a gloved finger into the rectum to check the part of the prostate next to the rectum. This is done to look for swelling or tenderness.
- Prostate massage. The healthcare provider massages your prostate gland to drain fluid into the urethra. This fluid is then checked under a microscope to look for inflammation or infection. This test is often done during a DRE.
- Semen culture. A semen sample is tested in the lab for bacteria and white blood cells.
- Cystoscopy. A thin, flexible tube and viewing device is put into the penis and through the urethra. Your healthcare provider uses the device to look at your bladder and urinary tract for structural changes or blockages.
- Transrectal ultrasound. A small, handheld device (transducer) is inserted into the rectum next to the prostate to show images of the prostate. Biopsies may be taken at this time.
- CT scan. This is an imaging test that uses X-rays and a computer to make detailed images of the body. A CT scan shows details of the bones, muscles, fat, and organs.
How is prostatitis treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment depends on what type of prostatitis you have.
Chronic prostatitis (chronic pelvic pain syndrome)
You may take antibiotics until infection can be ruled out. Depending on the symptoms, other treatments may include:
- Medicines to help relax the muscles around the prostate and bladder, decrease inflammation, and ease pain
- Prostate massage to release the fluid that is causing pressure in the prostate
- Heat from hot baths or a heating pad to help ease discomfort
Chronic bacterial prostatitis
Treatment often means taking antibiotics for 4 to 12 weeks. This type of prostatitis is hard to treat, and the infection may come back. If antibiotics don’t work in 4 to 12 weeks, you may need to take a low dose of antibiotics for a while. In rare cases, you may need surgery to remove part or all of the prostate. This may be done if you have trouble emptying your bladder.
Acute bacterial prostatitis
For this type of prostatitis, you often take antibiotics for 2 to 4 weeks. It’s important to take the full course of antibiotics, even when you don’t have symptoms. This is to stop the growth of antibiotic-resistant bacteria. You may also need pain medicines. You may be told to drink more fluids. In severe cases, you may need to stay in the hospital.
Always see your healthcare provider for more information about the treatment of prostatitis.
Key points about prostatitis
- Prostatitis is inflammation of the prostate gland caused by infection. It can be 1 of several types.
- Prostatitis is not contagious and is not a sexually transmitted infection (STI). But it can be caused by an STI.
- Prostatitis can happen at any age. Symptoms may include peeing more often, a burning or stinging feeling when peeing, pain peeing, and fever and chills.
- Your healthcare provider often diagnoses prostatitis by your symptoms and by checking your urine and semen for signs of infection.
- Antibiotics are used to treat prostatitis. In rare cases, you may need surgery.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new directions your provider gives you.
- Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions, especially after office hours or on weekends.
Benign Prostatic Hyperplasia
What is benign prostatic hyperplasia?
Benign prostatic hyperplasia (BPH) is also called benign prostatic hypertrophy. It’s when the prostate gland becomes very large and may cause problems passing urine. BPH is not cancer. It's a common part of aging.
The prostate gland is found only in males. It’s located in front of the rectum and below the bladder. It wraps around the urethra. This is the tube that carries urine out of the body. The prostate's job is to make some of the fluid that protects and nourishes sperm cells in semen. This makes the semen more liquid.
BPH can raise levels of PSA (prostate-specific antigen). PSA is a protein made by the prostate and can be measured with a blood test. Very little PSA is in the blood when the prostate is healthy. An increased PSA level does not mean you have cancer. But the higher the PSA level, the higher the chance of having cancer.
Some symptoms of BPH and prostate cancer are the same. But BPH is not cancer and does not develop into prostate cancer.
What causes BPH?
The cause of BPH isn't known. The prostate goes through 2 main periods of growth. In early puberty, it doubles in size. Then around age 25, the prostate starts to grow again. It continues to grow for most of a man's life.
The continuing growth of the prostate may not cause problems until much later in life, when the second period of growth may result in BPH. It is a common problem for men starting in their 60s. And it is more likely for men in their 70s and 80s to have some symptoms of BPH.
Risk factors may include obesity, a family history of BPH, being over age 40, physical inactivity, erectile dysfunction, heart disease, and type 2 diabetes.
What are the symptoms of BPH?
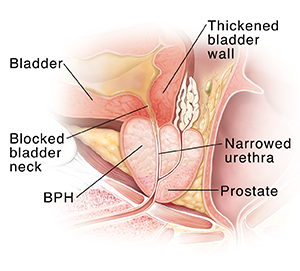
As the prostate grows, it presses against the urethra, the tube that carries urine out of the body. This interferes with urination. At the same time, the bladder wall becomes thicker and irritated, and begins to contract, even when it contains only small amounts of urine. This can cause more frequent urination. These changes cause the bladder muscle to weaken. It may not empty fully and can leave some urine behind. This leads to symptoms.
The following are the most common symptoms of BPH:
- Leaking or dribbling of urine
- Trouble starting urine stream
- More frequent urination, especially at night (nocturia)
- Urgency to urinate
- Holding urine (can't pass urine)
- An interrupted, weak stream of urine
These problems may lead to 1 or more of the following if BPH is not treated:
- Loss of urine control
- Kidney damage
- Blood in the urine
- Bladder damage
- Urinary tract infections
- Bladder stones
- Inability to pass urine at all
The symptoms of BPH may look like other conditions or health problems. Always talk with a healthcare provider for a diagnosis.
How is BPH diagnosed?
Diagnosing benign prostatic hyperplasia (BPH) in its earlier stages can lower the risk of complications. Your healthcare provider will review your health history and do a physical exam. Other tests may include:
- Urine tests. To check for infection.
- Digital rectal exam. A procedure where the healthcare provider puts a gloved finger into the rectum to feel the part of the prostate next to the rectum.
- Ultrasound (sonography). An imaging test that uses high-frequency sound waves to create images of the prostate and nearby organs on a computer screen.
- Cystoscopy. A thin flexible tube and viewing device (cystoscope) is put into the penis and through the urethra. It lets the healthcare provider look at the bladder and urinary tract for structure changes or blockages.
- Urine flow study. A test where the man urinates into a device that measures how quickly the urine is flowing. Reduced flow may suggest BPH.
- Post void residual. A test like an ultrasound that measures that amount of urine in the bladder after urination.
How is BPH treated?
With time, BPH symptoms often need some kind of treatment. When the prostate is just mildly enlarged, treatment may not be needed. In fact, research has shown that, in some mild cases, some of the symptoms of BPH get better without treatment. The need to start treatment will be decided by you and your healthcare provider after careful evaluation of your symptoms.
Active surveillance means that your provider will perform regular check-ups to watch for developing problems, but you will not have other treatments.
Treatment for BPH may include:
Surgery
To remove only the enlarged tissue that is pressing against the urethra (the tube that carries urine out of the body), with the rest of the inside prostate left intact. Types of surgery often include:
-
Transurethral surgery. No outside
cut (incision) is needed. The surgeon reaches the prostate by putting a tool
through the urethra.
- Transurethral resection of the prostate (TURP). A thin, narrow tube (resectoscope) is put into the urethra through the penis. The surgeon uses tools through the resectoscope to remove the prostate tissue blocking the urethra 1 piece at a time. The pieces of tissue are carried into the bladder. They are flushed out at the end of the surgery.
- Transurethral incision of the prostate (TUIP). A procedure that widens the urethra by making small cuts where the urethra joins the bladder (the bladder neck), and in the prostate gland itself.
- Laser surgery. Using laser tools to cut away the prostate tissue blocking the urethra. The laser fiber is passed through the urethra to the prostate.
- Open surgery. Surgery that needs an incision (cut) in the skin. This is often done when the gland is very big, when there are complicating factors, or when the bladder has been damaged and needs to be fixed.
Nonsurgical treatments
These may include:
- Transurethral microwave thermotherapy (TUMT). Microwaves are used to heat and destroy prostate tissue to reduce urinary frequency and urgency. A thin flexible tube is put into the urethra to get the microwaves to the right parts of the prostate.
- Medicines. These are used to shrink or at least stop the growth of the prostate without using surgery. Or to make the muscles around the urethra looser so urine flows more easily.
- Water-induced thermotherapy. Heated water is sent through a soft flexible tube into the urethra to heat and destroy prostate tissue.
- Urolift. Small stitches are placed into the sides of the prostate through a camera to pull the blocking prostate tissue open.
What are possible complications of BPH?
Delay in treatment can cause lasting (permanent) bladder damage that can't be treated.
Living with BPH
Management of BPH may include:
- Lifestyle factors. Limit fluids in the evening, empty your bladder before going to bed, and don’t take water pills (diuretics) that are active at night. Talk with your healthcare provider before changing the timing of your medicines. Losing weight and staying physically active may also help.
- Dietary factors. Stay away from or reduce the amount of alcohol, coffee, and other fluids. This is especially important after dinner. A higher risk for BPH has been linked to a diet high in zinc, butter, and margarine. Eating a healthy diet high in fruits and vegetables may also help.
- Don't use medicines that make symptoms worse. Decongestants and antihistamines can slow urine flow in some men with BPH. Some antidepressants and diuretics can also make symptoms worse. Talk with your healthcare provider if you are taking any of these medicines.
- Kegel exercises. Repeated tightening and releasing the pelvic muscles is called Kegel exercises. These can help prevent leaking urine. Practice these exercises while urinating to train the specific muscle. To do Kegels, contract the muscle until the flow of urine decreases or stops. Then release the muscle.
Key points about BPH
- BPH is when the prostate gland becomes very large and may cause problems passing urine.
- The cause of BPH is not known. Growth of the prostate may not cause problems until much later in life.
- As the prostate enlarges, it presses on the urethra. This causes symptoms, such as changes in urination.
- BPH may not need treatment. If needed, treatment includes medicines. It also includes various procedures and surgeries to remove the part of the prostate that’s pressing on the urethra.
- Management of BPH may include lifestyle changes, including dietary changes and specific exercises.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions. Ask how to contact your provider with urgent concerns on weekends, holidays, and after office hours.
Prostate Problems and Related Urinary Symptoms
Prostate Problems and Related Urinary Symptoms
BPH
BPH (benign prostatic hyperplasia) develops when changing hormone levels cause the prostate to grow larger. This often starts around age 50. Excess tissue can block the urethra, making it harder for urine to flow. The enlarged prostate can also press on the bladder, so you may need to urinate more often. Other symptoms include straining during urination, a weak urine stream, urinating more at night, incontinence, dribbling at the end of urination, and feeling that the bladder isn’t emptying all the way. Note that BPH is not cancer and does not cause cancer.
How BPH affects the bladder
Pushing to urinate through a narrowed urethra can cause the bladder walls to thicken or stretch out of shape. A stretched bladder may have problems emptying all the way. If urine stays in the bladder longer than it should, you may develop an infection or bladder stones. Also, the kidneys can’t drain properly into a bladder that doesn’t empty completely. This can lead to kidney failure. Pressure from urine buildup can also cause leaking of urine (called overflow incontinence).
Other prostate problems
Prostatitis is an infection or inflammation that causes the prostate to become painful and swollen. The swelling narrows the urethra and can block the bladder neck. Prostatitis can cause a burning sensation during urination. You may also feel pressure or pain in the genital area. In some cases, prostatitis can cause fever and chills, and can make you very sick.
Cancer occurs when abnormal cells form a tumor (a lump of cells that grow uncontrolled). Some tumors can be felt during a physical exam, others can’t. Prostate cancer often causes no symptoms at all, especially in its early stages. Prostate symptoms are more likely to be caused by a problem that is NOT cancer.