Understanding Endoscopic Magnetic Esophageal Sphincter Augmentation
Endoscopic magnetic esophageal sphincter augmentation, or magnetic sphincter augmentation (MSA), is surgery used to treat GERD (gastroesophageal reflux disease). It's a minimally invasive approach used to prevent stomach contents from coming back up into the esophagus and causing heartburn.
Understanding GERD
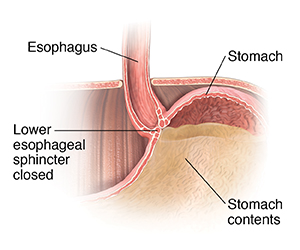
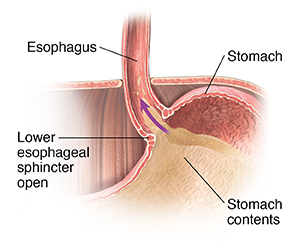
When you eat, food travels from your mouth down a tube called the esophagus to your stomach.Along the way, food passes through the lower esophageal sphincter (LES). This is a ring of muscle that acts as a 1-way valve. Normally, the LES opens when you swallow. It allows food to enter the stomach. Then it closes completely and quickly. It is natural for the LES to open when you belch to let air come up. When you have GERD, the LES doesn’t work well enough to hold food and fluids in the stomach. Food and fluid back up into the esophagus, causing heartburn and other symptoms.
MSA uses a device placed over the lower end of the esophagus, near the LES. The device is made up of magnets. Each magnet is covered in titanium and wired together in a ring. The magnets let the ring get bigger or smaller, almost like a rubber band. When you swallow, the pressure increases at the LES. The LES opens and the ring stretches open to allow food and fluids to get to the stomach. Once the food reaches the stomach, the pressure drops and the LES closes. The MSA ring then also closes. This helps keep the LES closed and helps prevent the reflux of stomach contents into the esophagus.
Why MSA is done
Left untreated, GERD can get worse and lead to serious problems over time. GERD can cause pain, bleeding, and trouble swallowing. It can also raise your risk for cancer of the esophagus.
If lifestyle changes and medicines don't help your symptoms, you may need surgery. MSA is 1 type of surgery that may be used.
Your provider will order other tests first to make sure MSA is the right procedure for you.
How MSA is done
MSA surgery is done using laparoscopy. This approach uses a thin, lighted tube called a laparoscope (scope). In general, here’s what happens:
- First, you will be asked to sign an informed consent. Signing this form means you understand both the risks and benefits of the procedure. It also means you've been informed of alternative treatments and that your questions have been answered. Be certain to ask all your questions before singing the form.
- You’ll have an IV (intravenous) line put in to give you fluids and medicines.
- You’ll also be given anesthesia that keeps you free from pain during the surgery. You may be drowsy but awake. Or you may be in a deep sleep-like state through the surgery.
- The surgeon will make several small cuts (incisions) in the belly. The scope will be put through 1 incision. Surgical tools will be placed through the other incisions.
- Your belly (abdomen) will be filled with carbon dioxide (CO2) gas. This gives the surgeon more space to see and work.
- The surgeon will measure the area where the device will be placed. They will choose the correct size of the device.
- The surgeon will place the device around the esophagus and connect the ends.
- The CO2 gas and all surgical tools will be removed after surgery.
- The incisions will be closed with stitches or surgical tape.
You will be taken to the recovery room, where you will be closely watched. You may go home the same day. Or you may stay overnight in the hospital. You can go home when your condition is stable, you can keep fluids down, and you can urinate. Because you had anesthesia, have an adult family member or friend drive you home.
Risks of MSA
Risks of MSA may include:
-
Trouble swallowing if the LES doesn't relax. This often goes away after a few weeks.
-
Wearing away of the deviceinto the esophagus. In this case, the device may need to be removed.
-
Bloating
-
Diarrhea or constipation
-
Problems related to anesthesia
- Allergic reactions. You should not have the procedure if you are allergic to titanium, nickel, zinc, or stainless steel.
- Infection after the surgery