Nerve Injuries
When you choose Saint Luke's, you benefit from team-based, compassionate care. Our neurosurgeons work with plastic and reconstructive surgeons, neurologists, and therapists to offer comprehensive treatment for nerve injuries and disorders.
Carpal Tunnel Syndrome
What is carpal tunnel syndrome?
Carpal tunnel syndrome is a condition that causes problems in your hand and wrist. It happens when the median nerve is squeezed (compressed) as it passes through the carpal tunnel. The carpal tunnel is an opening inside your wrist. It is formed by the carpal (wrist) bones underneath the median nerve and the transverse carpal ligament across the top of the median nerve. The median nerve provides sensory and motor functions to the thumb and three middle fingers. If it gets compressed or irritated, you may have symptoms.
What causes carpal tunnel syndrome?
Most cases of carpal tunnel syndrome have no specific cause. Things that may be part of the cause include:
Frequent, repetitive, small movements with the hands, such as typing or using a keyboard.
Frequent, repetitive, grasping movements with the hands, such as with sports and certain physical activities.
Joint or bone disease. Examples are arthritis, osteoarthritis, and rheumatoid arthritis.
Hormonal or metabolic changes. Examples are menopause, pregnancy, and thyroid imbalance.
Changes in blood sugar levels, like with type 2 diabetes.
Other conditions or injuries of the wrist. Examples are strain, sprain, dislocation, break, and swelling and inflammation.
Family history of carpal tunnel syndrome.
Who is at risk for carpal tunnel syndrome?
Women get carpal tunnel syndrome 3 times more often than men. The risk increases during pregnancy. It generally occurs only in adults. You may be at risk if you have an underlying health problem, such as diabetes or kidney failure. These conditions put you at risk for nerve compression, including carpal tunnel syndrome.
What are the symptoms of carpal tunnel syndrome?
The most common symptoms include:
Weakness when gripping objects with one or both hands.
Pain or numbness in one or both hands.
"Pins and needles" feeling in the fingers.
Swollen feeling in the fingers.
Burning or tingling in the fingers, especially the thumb and the index and middle fingers.
Pain or numbness that is worse at night, interrupting sleep.
The symptoms of carpal tunnel syndrome may seem like other health conditions or problems. Always see your doctor for a diagnosis.
How is carpal tunnel syndrome diagnosed?
Your doctor will check your health history and give you a physical exam. They may advise electrodiagnostic tests on your nerves. These tests are also known as nerve conduction studies and electromyography. They are the best way to diagnose carpal tunnel syndrome. The tests stimulate the muscles and nerves in your hand to see how well they work. Ultrasound can also diagnose carpal tunnel in many people.
How is carpal tunnel syndrome treated?
Your doctor will discuss different treatment choices with you. Treatment will depend on your symptoms, age, and general health. It will also depend on how bad the condition is.
Treatment may include:
Splinting your hand. This helps keep your wrist from moving. It also eases the compression of the nerves inside the tunnel.
Anti-inflammatory medicines. These are taken by mouth (oral) or injected into the carpal tunnel space. These ease the swelling.
Work area changes. Changing the position of your computer keyboard or making other ergonomic changes can help ease symptoms.
Exercise. Stretching and strengthening exercises can help when your symptoms are better. A physical or occupational therapist may watch you do the exercises. Yoga can also help.
Surgery. You may need surgery if the condition doesn’t get better with other treatments or go away on its own. This surgery is called carpal tunnel release. This eases compression on the nerves in the carpal tunnel.
Key points about carpal tunnel syndrome
Carpal tunnel syndrome happens when the median nerve is squeezed (compressed) as it passes through the carpal tunnel in the wrist.
Women get carpal tunnel syndrome 3 times more often than men. It generally occurs only in adults.
Symptoms include weakness when gripping objects, pain or numbness in hands, and a “pins and needles” feeling in the fingers.
To diagnose carpal tunnel syndrome, you may have electrodiagnostic tests. These tests stimulate the muscles and nerves in your hand to see how well they work.
Treatment may include splinting your hand, medicines, work area changes, exercise, or surgery.
Next steps
Tips to help you get the most from a visit to your doctor:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your doctor tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new directions your doctor gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your doctor if you have questions, especially after office hours or on weekends.
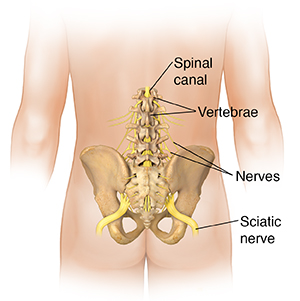
Sciatica
What is sciatica?
Sciatica, also called lumbar radiculopathy, is a pain that originates along your sciatic nerve. It's a symptom of an underlying condition, not a diagnosis. The sciatic nerve extends from the back of your pelvis down the back of your thigh. Your sciatic nerve is the main nerve in your leg. It's also the largest nerve in your entire body.
What causes sciatica?
Usually, sciatica is caused by a herniated (or bulging) disk in your spine that presses on your sciatic nerve.
Other reasons for pressure on your sciatic nerve may include:
- Obesity
- Poor posture
- Tumor
- Abscess
- Blood clot
- Awkward sitting position
- Any nerve disorders
Health conditions, such as diabetes or Lyme disease, can cause symptoms of sciatica. Sometimes, the cause for your sciatica can't be identified.
What are the symptoms of sciatica?
These are the most common symptoms of sciatica:
- Lower back pain that radiates or spreads down your buttock and the back of one thigh
- Pain that extends from your buttock down to your foot
- Numbness (in severe cases)
- Weakness (in severe cases)
The symptoms of sciatica may look like other conditions or health problems. Always see your healthcare provider for a diagnosis.
How is sciatica diagnosed?
Along with a complete medical history and physical exam, tests for sciatica may include:
- X-ray. Electromagnetic energy beams make images of internal tissues, bones, and organs onto film.
- MRI. Large magnets, radio waves, and a computer make detailed images of organs and structures in your body.
- Electromyography and nerve conduction study (EMG and NCS). A procedure done together to record and analyze electrical impulses in your muscles. During the EMG, thin needles are placed in your muscle to record electrical activity. The NCS is often done along with the EMG to determine if a nerve is working normally. Electrodes are then placed in various locations on your skin along the nerve pathway. When stimulating the nerve at various places, your healthcare provider can then find the specific site of your injury.
- Myelogram. This is an invasive procedure that uses a special dye (contrast material) to be injected through a needle into the spinal canal. The dye helps any deformities to show up on X-rays. This procedure is normally only done when other tests don't find the cause of the symptoms.
How is sciatica treated?
Sciatica usually heals on its own with some rest, appropriate movement, and time.
Physical activity is important. Don’t stay in bed. Lack of movement will cause problems in other parts of your body.
Find a comfortable position, but stay as active as you can. As strange as it may seem, appropriate motion helps to reduce inflammation and pain. Talk to you healthcare provider about when to start stretching exercises so you can resume regular physical activities without pain. Your provider may suggest short walks or physical therapy.
To help relieve the pain, treatment may include:
- Nonsteroidal anti-inflammatory drugs, (NSAIDs) such as ibuprofen
- Heat or cold applied to the sore muscles
- Specific stretching exercises or physical activities (motion reduces inflammation)
- Osteopathic manipulation
- Surgery (to fix your herniated disk, if the condition persists)
What are possible complications of sciatica?
Because sciatica is caused by pressure on a nerve in your spine, complications may develop if the pressure is not relieved. Possible complications of unrelieved nerve compression include:
- Increased pain
- A slipped or herniated disc
- Loss of feeling or weakness in your affected leg
- Loss of bowel or bladder function
- Permanent nerve damage
When should I call my healthcare provider?
Call your healthcare provider if:
- You develop back pain when you have a history of cancer.
- You have a high fever.
- Your pain gets worse.
- You lose feeling in your affected leg or notice weakness in your leg.
- You develop problems with your bowels or bladder.
- Your pain returns after successful treatment of your sciatica.
Key points about sciatica
- Sciatica most commonly occurs in people between the ages of 30 and 50 years.
- It's pain that starts along your sciatic nerve and spreads down your buttock and the back of one thigh.
- It's usually caused by a herniated (or bulging) disk in your spine that presses on your sciatic nerve.
- Sciatica usually heals on its own with some rest, appropriate exercise, and time.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.
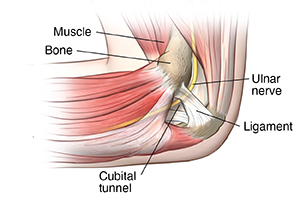
Cubital Tunnel Syndrome
What is cubital tunnel syndrome?
Cubital tunnel syndrome happens when the ulnar nerve, which passes through the cubital tunnel (a tunnel of muscle, ligament, and bone) on the inside of the elbow, becomes inflamed, swollen, and irritated.
Cubital tunnel syndrome causes pain that feels a lot like the pain you feel when you hit the "funny bone" in your elbow. The "funny bone" in the elbow is actually the ulnar nerve, a nerve that crosses the elbow. The ulnar nerve starts in the side of your neck and ends in your fingers.
What causes cubital tunnel syndrome?
Cubital tunnel syndrome may happen when a person bends the elbows often (when pulling, reaching, or lifting), leans on their elbow a lot, or has an injury to the area.
Arthritis, bone spurs, and previous fractures or dislocations of the elbow can also cause cubital tunnel syndrome.
In many cases, the cause is not known.
What are the symptoms of cubital tunnel syndrome?
The following are the most common symptoms of cubital tunnel syndrome:
Numbness and tingling in the hand or ring and little finger, especially when the elbow is bent
Numbness and tingling at night
Hand pain
Weak grip and clumsiness due to muscle weakness in the affected arm and hand
Aching pain on the inside of the elbow
The symptoms of cubital tunnel syndrome may seem like other health conditions or problems, including golfer's elbow (medial epicondylitis). Always see a healthcare provider for a diagnosis.
How is cubital tunnel syndrome diagnosed?
In addition to a complete medical history and physical exam, diagnostic tests for cubital tunnel syndrome may include:
Nerve conduction test. This test measures how fast signals travel down a nerve to find a compression or constriction of the nerve.
Electromyogram. This test checks nerve and muscle function and may be used to test the forearm muscles controlled by the ulnar nerve. If the muscles don't work the way they should, it may be a sign that there is a problem with the ulnar nerve.
X-ray. This is done to look at the bones of the elbow and see if you have arthritis or bone spurs in your elbow.
How is cubital tunnel syndrome treated?
The most effective treatment for cubital tunnel syndrome is stopping the activity that is causing the problem. Treatment may include:
Resting and stopping any activity that aggravates the condition, such as bending the elbow
A splint or foam elbow brace worn at night (to limit movement and reduce irritation)
Using an elbow pad (to protect against chronic irritation from hard surfaces)
Anti-inflammatory medicines (such as ibuprofen or naproxen)
Nerve gliding exercises
If these treatments don't work, the healthcare provider may talk to you about surgery.
What can I do to prevent cubital tunnel syndrome?
To prevent cubital tunnel syndrome:
Keep your arms flexible and strong.
Don't rest on your elbows, especially on a hard surface.
Warm up before exercising or using your arms for sports or other repetitive movements.
When should I call my healthcare provider?
Call your healthcare provider if you have:
Pain or trouble moving that affects your regular daily activities
Pain doesn’t get better or gets worse with treatment
Numbness, tingling, or weakness in the arm or hand
Key points about cubital tunnel syndrome
Cubital tunnel syndrome is a problem with the ulnar nerve, which passes through the inside of the elbow. It causes pain that feels a lot like the pain you feel when you hit the "funny bone" in your elbow.
Cubital tunnel syndrome may happen when a person frequently bends the elbows, leans on their elbow a lot, or has an injury to the area. Arthritis, bone spurs, and previous fractures or dislocations of the elbow can also cause it. In many cases, the cause is not known.
The most common symptoms of cubital tunnel syndrome are numbness, tingling, and pain in the hand or ring and little finger, especially when the elbow is bent.
Cubital tunnel syndrome can be treated with rest and medicines to help with pain and inflammation. Exercises may help, too. In some cases, surgery may be done.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your healthcare provider if you have questions, especially after office hours or on weekends and holidays.
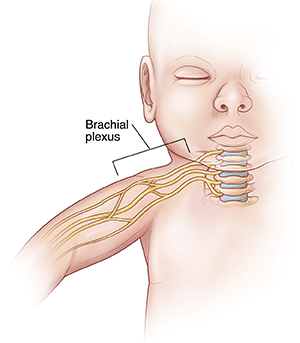
Brachial Plexus Injuries
What is a brachial plexus injury?
The brachial plexus is a bundle of connected nerves in the neck region coming from your spine. It branches under the clavicle (collarbone) down into your chest, shoulders, arms, and hands. This group of nerves controls the motions of your shoulder, wrists, hands, and arms. The nerves let you do things like raise your arm, type on your keyboard, and throw a baseball.
The brachial plexus nerves are sensory, too. For example, they let you know that a pan you grab with your hand is too hot to hold.
The brachial plexus can be injured in many different ways from pressure, stress, or being stretched too far. The nerves may also be damaged by cancer or radiation treatment. Brachial plexus injuries can happen to babies during childbirth. In some cases, an overactive immune system can damage the plexus.
Brachial plexus injuries cut off all or part of the communication between the spinal cord and the arm, wrist, and hand. This may mean that you can't move or feel parts of your arm or hand. Often, brachial plexus injuries cause pain or a total loss of feeling in the area.
The severity of a brachial plexus injury varies. In some people, function and feeling returns to normal. Others may have lifelong disability because they can't use or feel a part of the arm.
Brachial plexus injuries are categorized as type:
Avulsion. The root of the nerve is completely separated from the spinal cord (the most severe type).
Neurapraxia. The nerves are stretched (the least severe type).
Rupture. Part of the nerve is actually torn.
Neuroma. Scar tissue forms on the stretched nerve as it fixes itself.
Brachial neuritis. This is a rare syndrome for which no cause can be identified. It's also called Parsonage-Turner syndrome.
Brachial plexus birth injury happens when the brachial plexus gets stretched during childbirth. It is called Erb palsy or Klumpke palsy, depending on which part of the plexus is injured. Erb palsy affects 1 or 2 babies in every 1,000 births.
What causes a brachial plexus injury?
The most common cause of this injury is when the neck is tilted while pulling (traction) happens on the other side of the neck. But the causes of injury vary, including motor vehicle accidents, falls, gunshot wounds, athletic injuries (especially contact sports), and childbirth.
During childbirth, large babies may be at an increased risk for brachial plexus injuries. A quick or emergency delivery, when the baby must be forcibly pulled out, can cause a brachial plexus injury. This happens because the baby's neck is often flexed severely in one direction. Babies in breech position (bottom end comes out first) and those whose labor lasts an unusually long time may also suffer brachial plexus injuries.
Cancer and radiation therapy can cause brachial plexus injury. The tumor itself can invade the brachial plexus. Radiation of lymph nodes in the area can also damage the nerves.
Autoimmune disorders can sometimes cause the immune system to attack the plexus.
Who is at risk for a brachial plexus injury?
Factors that may raise your risk are:
Motor vehicle accidents.
Sports activities, especially football.
Childbirth, especially large babies, breech position, or long labor.
Cancer and radiation therapy.
What are the symptoms of a brachial plexus injury?
Symptoms depend on where along the length of the brachial plexus the injuries happen and how severe they are.
Common symptoms of brachial plexus injuries are:
No feeling in the hand or arm.
Pain in the arm or hand.
Inability to control or move the arm, wrist, or hand.
An arm that hangs limply.
How is a brachial plexus injury diagnosed?
A doctor will examine your hand and arm. They will test for feeling and function to help diagnose this type of injury.
Other diagnostic tests include:
Imaging tests, such as an ultrasound (sonogram), MRI, or CT scan.
Tests to determine nerve function and electrical activity, including a nerve conduction study and electromyogram.
X-ray of the neck and shoulder area.
How is a brachial plexus injury treated?
Some brachial plexus injuries need surgery to repair the damage. Physical therapy can help you restore function in your arms and hands. It can also improve range of motion and flexibility in stiff muscles and joints.
Brachial plexus injuries don't always need treatment. Some people, especially babies with a brachial plexus birth injury, get better without any treatment. But it can take as long as several months for the injury to heal. Certain exercises can help with healing and function.
You may need regular checkups to watch the progress and healing of a brachial plexus injury. Checkups are especially important for babies. They may be needed for as long as 2 years as the injury heals.
In some cases, a surgeon can connect other nerves or tendons to the muscles of the arm or hand to restore function. This is only done when the chance of spontaneous nerve growth becomes unlikely.
Medicine may be used if your doctor thinks you may have an autoimmune condition.
What are possible complications of a brachial plexus injury?
Brachial plexus injuries often heal well if they aren't severe. Many people with minor brachial plexus injuries recover between 90% and 100% of the normal function of their arms.
For severe brachial plexus injuries, surgery may be needed right away to try to get function back. Without it, you might have a lasting disability and be unable to use your arm or hand.
If you have a brachial plexus injury that causes a lack of feeling, you must take special care when dealing with hot items, razors, knives, or other objects that could harm you. A brachial plexus injury can keep you from feeling any other injury to the affected area. You may not notice that you're hurt.
You may also have long-term pain or sensory changes in the affected area. Or you could have paralysis.
What can you do to prevent a brachial plexus injury?
To help prevent these injuries:
Develop safe driving habits.
Maintain good body mechanics during sports activities and use safety gear.
When to contact your doctor
If you have had an injury to the neck or shoulder area and you can't feel or move your hand or arm, contact your doctor to find out what's causing your symptoms. Get assessed and diagnosed right away to help prevent permanent damage.
Key points about brachial plexus injury
The brachial plexus is a bundle of connected nerves in the neck region coming from your spine. This group of nerves controls the motions of your shoulder, wrists, hands, and arms.
Brachial plexus injuries cut off all or part of the communication between the spinal cord and the arm, wrist, and hand. This may mean that you can't move or feel parts of your arm or hand.
The most common cause of this injury is when the neck is tilted while pulling (traction) happens on the other side of the neck. But the causes of injury are varied.
Some brachial plexus injuries need surgery to repair the damage. Physical therapy can help you restore function in your arms and hands.
Get assessed and diagnosed right away to help prevent permanent damage.
Next steps
Tips to help you get the most from a visit to your doctor:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your doctor tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your doctor gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your doctor if you have questions, especially after office hours or on weekends and holidays.
Locations

Saint Luke's Neurological & Spine Surgery–Plaza