Heart Attack
A heart attack, also known as acute myocardial infarction (AMI) is what happens when blood cannot get to part of the heart muscle. Part of the heart muscle then begins to die. A heart attack can be deadly. It is vital to get help as soon as possible.
Chest pain is the most common symptom of a heart attack. You may feel the pain in only one part of your body, or it may move from your chest to your arms, shoulder, neck, teeth, jaw, belly area, or back. If you have symptoms of a heart attack, call 911 right away and get to a Saint Luke’s Health System hospital fast.
Every minute counts during a heart attack. The Emergency Departments at each of our hospitals provide protocol-driven chest pain management. Our clinicians use time-saving measures to ensure patients having a heart attack receive critical cardiac care—including lifesaving emergency angioplasty—as quickly as possible.
Saint Luke's Hospital, Saint Luke's East Hospital, Saint Luke's North Hospital, and Saint Luke's South Hospital have all earned U.S. News and World Report "Best Hospitals" as High Performing hospitals in Heart Attack.
Saint Luke's Hospital has received the Get With The Guidelines Mission Lifeline: Gold Plus Target: STEMI Receiving Award from the American Heart Association.
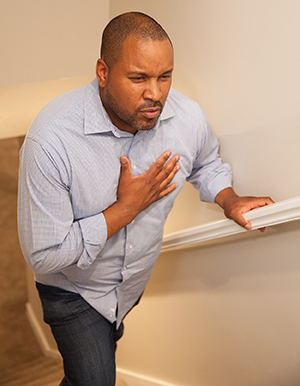
Symptoms
Symptoms of a Heart Attack
A heart attack is also known as acute myocardial infarction, or AMI. It's an urgent message from your heart that it’s starved for oxygen. When a clot blocks a blood vessel feeding the heart (coronary artery), oxygen-rich blood can’t reach a part or all of your heart. Then tissues of the heart muscle start to die. This causes symptoms of a heart attack. The sooner you get to the hospital, the sooner treatment can start to help save your life and your heart.
Warning signs of a heart attack

-
Chest discomfort. With most heart attacks, there's discomfort in the center of the chest. This can last more than a few minutes. Or it can go away and come back. It can feel like uncomfortable pressure, squeezing, burning, fullness, tightness, or pain. It's often described as something heavy sitting on your chest.
-
Discomfort in other parts of the upper body. Symptoms can include pain or discomfort in 1 or both arms, shoulders, the back, neck, jaw, or stomach.
-
Shortness of breath. This may occur with or without chest discomfort.
-
Other signs. These may include breaking out in a cold sweat, upset stomach (nausea), or feeling lightheaded.
For women
Like men, women most often have chest pain or discomfort as a heart attack symptom. But women are a little more likely than men to have some of the less common symptoms. These include:
- Shortness of breath
- Abnormal tiredness
- Lightheadedness
- Heartburn
- Nausea and vomiting
- Back pain
- Jaw pain
For older adults
Older adults may also have different symptoms. These include:
- Fainting (syncope)
- Weakness
- Confusion (delirium)
For people with diabetes
If you have diabetes, high blood sugar can damage nerves in your body over time. This may keep you from feeling pain caused by a heart problem, leading to a “silent” heart problem. If you don’t feel symptoms, you're less able to get treatment right away. Talk with your healthcare provider about how to lower your risk for silent heart problems.
Call 911
Don’t be afraid to call 911, even if you’re not sure you're having a heart attack. If you don’t know the cause of your symptoms, assume it’s a heart attack. Play it safe and call 911 right away. Don't drive yourself to the emergency room (ER).
If you think someone else is having a heart attack, call 911 right away instead of driving them to the ER. After you call 911, they'll tell you what to do. The 911 dispatcher may tell you to give the person aspirin while waiting for help to arrive. If the dispatcher doesn’t tell you to do this, don't give the person aspirin. Aspirin can be dangerous in certain cases.
When you've had a past heart attack
People who've had one heart attack are at risk of having another. Your healthcare provider may prescribe medicine such as nitroglycerin to take for chest pain. You may also need medicine to lower your heart rate and blood pressure. This is to prevent angina and another heart attack. Remember to take any medicines your provider has given as directed. Don't stop these medicines without talking with them first.
Warning Signs
Warning Signs of Heart Attack
Since you’ve had a heart attack, your risk of having another is increased. Before you leave the hospital, ask your healthcare provider what symptoms to watch for. The list below may help. Keep in mind that the symptoms of a second heart attack may feel a lot like the symptoms of the first one. But they can also feel completely different. Also remember that women may have some symptoms that are different from men.
The faster you get help during a heart attack, the less damage to your heart. If you think you’re having another heart attack, call 911right away. Signs of a heart attack may include:
-
Pressure, squeezing, discomfort or pain in the chest
-
Other mild pain or discomfort in the neck, jaw, shoulders, arms, or back
-
Shortness of breath
-
Dizziness or faintness
-
Upset stomach (nausea) or vomiting
-
Sweating
If you have diabetes, your symptoms may be very mild. Or you may not even have warning symptoms at all.
To learn more
Living Well After a Heart Attack
Living Well After a Heart Attack
Recovery from a heart attack may take a few months. As you slowly get better, stick to the lifestyle changes you have made. Don’t go back to the same old habits. They may have led to your heart attack. After a heart attack, you are likely to be prescribed some new medicines. Some medicines help prevent future clots that could lead to another heart attack. Other medicines treat other conditions such as high blood pressure and high cholesterol. Take your medicines. And stick to the changes you’ve made to improve your heart and overall health. Here are more ways to help you live well after a heart attack.
Follow up with your provider

See your healthcare provider for follow-up visits as directed. During these visits, your provider will ask you about your medicines and how well they are working. If needed, your provider may change your dosage or prescribe new medicines. You may have tests done again. These can include blood tests, ECGs, or exercise stress tests. If you have questions, keep a list. Ask them during these visits.
Take care of yourself
-
Don’t push yourself. You may feel better. But listen to your body. Don’t push yourself too hard or too fast. If you go back to work, think about going part-time at first.
-
Build in some stress breaks. Every few hours, stop what you’re doing. Do some deep breathing or visualization.
-
Get enough sleep. This is even more important after a heart attack. Sleep helps your body heal.
-
Stay alert for signs of another heart attack. Get help right away if you think you’re having another heart attack. The sooner you get treatment, the less damage will be done to your heart.
-
Keep your new good habits. Be mindful of the good habits you've learned. Don't go back to your past unhealthy lifestyle.
Rely on your supports
-
Friends, family, and coworkers may want to help. But they likely don’t know how. Be honest about your heart attack. And tell them practical ways they can help out.
-
Tell friends, family, employers, and coworkers about limitations you have.
-
Encourage friends and coworkers to share lunchtime walks and healthy snacks with you.
-
Pick a few close friends to encourage you. This can be helpful if you have trouble with the changes you’re making.
-
Keep using support groups or heart rehab programs. These give ongoing support and structure. This can help you keep your heart-healthy changes for good.
-
Use your resources to help you stick to your new lifestyle. This will let you make changes that last.
For family and friends
Your loved one will have ups and downs. That’s normal. Help them focus on the positive. Sticking to lifestyle changes will help them feel better and be healthier. Think about making the same changes, too. That can help your loved one make and keep these new healthy habits. Always talk about your concerns with your loved one. Keep the conversation open.
Leaving the Hospital
Heart Attack: Leaving the Hospital
Once you are discharged from the hospital, your recovery will continue at home. How long it takes to recover depends on several things. These include how much damage the heart attack caused, what complications occurred, and what treatments you had. When you leave the hospital, you’ll get instructions on how to care for yourself at home. Be sure you have all the information you need. You will likely leave the hospital with new medicines that may include aspirin, cholesterol-lowering medicine, and medicine that helps lower blood pressure and lessen the stress placed on your heart. These medicines are to help prevent another heart attack in the future. Making changes in your lifestyle to include heart healthy habits will also be important. These may include quitting smoking, eating a heart healthy diet, doing regular aerobic exercise, lowering your stress level, and getting proper rest.

Questions for your healthcare provider
Before you leave the hospital, make sure to know the answers to these questions:
-
When should I schedule my first follow-up appointment? How often are these appointments needed?
-
What medicines do I need and how do I take them? When do I need to come back to have these checked or readjusted, if necessary?
-
What further tests do I need?
-
What symptoms should I watch for? What are the signs and symptoms of a condition that needs immediate attention? Does this mean call my healthcare provider, or call 911?
-
How soon can I start a cardiac rehab program?
-
When can I return to work? When can I drive? Be active? Have sex?
-
How can I get help managing payment for my medical care?
Joining a cardiac rehab program
Cardiac rehabilitation (rehab) helps you recover after a heart attack. This program helps you learn how to make changes to improve your health and reduce your chances of having another heart attack. You might start an inpatient program while you’re in the hospital. If not, ask your healthcare provider about finding a program to join after you leave the hospital.
First Aid
First Aid: Heart Attacks
A heart attack (myocardial infarction, or AMI) is an emergency. It can happen suddenly from a blockage or sudden narrowing of your arteries. This reduces blood flow to your heart muscle. It's the result of years of damage to your blood vessels. Over time, fatty substances collect on the walls of the heart's arteries. This is from your genes and lifestyle choices. Many of these can lead to chronic disease. The arteries become narrower as the deposits build up within the artery walls. A heart attack can happen once one of these arteries narrows enough to stop oxygen supply to an area. It can also happen if the buildup breaks open and forms a blood clot.
Step 1. Call 911 NOW!
-
Call 911 for emergency medical services. Getting care right away may keep the heart from stopping. It may help limit damage to the heart muscle to a minimum.
-
When a heart attack is suspected, have the person chew 1 adult dose or 2 low-dose (baby) aspirin tablets. If you are not sure the chest pain is from a heart attack, this can be delayed until the emergency medical services arrive. If the person has been prescribed nitroglycerin, follow instructions from the provider for taking these tablets.
Step 2. Keep the heart attack victim calm
-
Have the victim stop all activities.
-
Reassure the victim. This will keep them calm, so the heart uses less oxygen.
-
Loosen any clothing that may restrict breathing. This includes ties, collars, and belts.
Step 3. Monitor the heart attack victim
-
Start CPR right away if the person shows signs that they have stopped breathing. Or start it if they are becoming unresponsive, or their pulse has stopped.
-
Do CPR by pushing down hard and fast in the center of the chest. Try to allow the chest to recoil or completely expand in between each compression. The goal is to push 100 to 120 times per minute. Emergency dispatchers on the telephone can give instructions on doing CPR.
-
Don't worry about doing rescue breaths during CPR. But if you have the training or are able to do rescue breaths, the goal is to provide 2 breaths for every 30 compressions. Rescue breaths also have been called mouth-to-mouth resuscitation.
-
Continue CPR until emergency professionals arrive. Or continue until the heart attack victim starts to move.
Warning signs of heart attack
The warning signs of a heart attack can include any of these:
-
Chest pain or constriction. This feels like pressure or a belt squeezing the chest.
-
Heaviness in the chest area. This is as if a heavy weight is resting on the chest.
-
Heaviness or pain going to the arms, shoulders, jaw, or teeth
-
Shortness of breath
-
Pale or gray skin tone and sweating. Also cool, damp skin.
- Feeling dizzy or lightheaded with no other cause
-
Feeling nauseated
-
Symptoms don't go away after taking heart medicine or nitroglycerin
-
Feeling heartburn or indigestion
