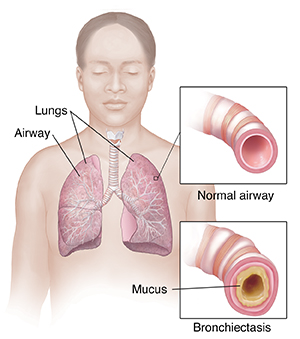
Understanding Bronchiectasis
Bronchiectasis is a condition in which the lungs' airways (the bronchi and bronchioles) are damaged and become wider than normal. Over time, the walls of the airways become thick and scarred. The damaged airways can’t clear mucus as well. Because of this, mucus builds up in the airways. This increases the risk for lung infections. Bronchiectasis is a long-term (chronic) condition.
What causes bronchiectasis?
Some causes of bronchiectasis are well understood, but others are not. Bronchiectasis can be present at birth (congenital), or it may happen later in life (acquired). It can occur at any age. It also occurs in people with lung infections who have long-term damage to the airways from other health problems.
Smokers and those with long-term lung disease are more likely to develop bronchiectasis. Some of the conditions that increase the chance for bronchiectasis include:
-
Cystic fibrosis
-
Lung infections, such as pneumonia, tuberculosis, infections related to it, or whooping cough
-
Chronic obstructive pulmonary disease (COPD)
-
Problems with the body’s disease-fighting (immune) system
-
Allergic bronchopulmonary aspergillosis (ABPA)
-
Long-term problem with inhaling food or liquids into the lungs (aspiration)
-
Certain autoimmune diseases, such as rheumatoid arthritis, Sjögren syndrome, and Crohn’s disease
- Disorders that affect cilia function, such as primary ciliary dyskinesia
-
Blocked airway, such as from a tumor or inhaled object
-
Lung problems that are present at birth (congenital)
What are the symptoms of bronchiectasis?
Damage to the airways often starts in childhood. You may not have symptoms until months or years after repeated lung infections. Some people have few or no symptoms. Others have daily symptoms that get worse over time. Common symptoms include:
-
Long-term cough that occurs daily and lasts over months or years
-
Coughing up a lot of thick mucus that may have blood, trapped particles, and pus in it
-
Trouble breathing, including shortness of breath and a whistling sound when you breathe (wheezing)
-
Inflammation of the nose and sinuses (rhinosinusitis)
-
Inflammation of the covering of the lungs (pleurisy or pleuritis)
-
Feeling tired
-
Chest pain
- Fever or chills
-
Flesh under fingers and toes gets thicker (clubbing)
-
Weight loss or abnormal growth rate in children
How is bronchiectasis diagnosed?
Your healthcare provider will ask about your past health and symptoms. You’ll also have a physical exam. This includes listening to your chest with a stethoscope. You may need tests to help with the diagnosis, including:
-
Blood tests. These check for infection, immune system problems, and overall health.
-
Sputum culture. This is a test of the mucus in your lungs. It’s checked for a bacterial or fungal infection.
-
Chest X-ray. This is done to get information about your heart and lungs.
-
Chest CT scan. This gives more detailed X-ray pictures of your airway. It’s most often used to make the diagnosis.
-
Lung function and exercise tests. They include spirometry and a 6-minute walk test. These tests show how well your lungs work and if you are able to get enough oxygen into your body, even when exerting yourself.
-
Sweat test. This or other tests may be done to diagnose cystic fibrosis.
-
Bronchoscopy. Sometimes, your provider may need to take a sample of mucus directly from the lungs. They will use a flexible tube (scope). The scope is placed into your mouth or nose and into your airways.