When Your Child Has a Fracture: Treatment with External Fixation
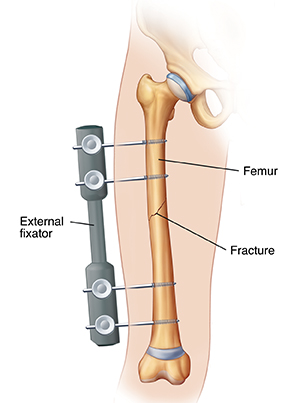
When your child’s bone is broken (fractured), the broken ends of the bone may need to be held together so the bone can heal. External fixation is a method of holding a fractured bone securely in place. It is not often needed for broken bones in children. But it might be needed for more severe breaks that are hard to treat with other methods. External fixation is put into place during surgery. An orthopedic surgeon (a surgeon who specializes in bone and joint problems) will do the procedure. The surgeon can discuss the procedure with you and answer your questions.
What is external fixation?
During external fixation surgery, metal pins or screws are put into bone on either side of the fracture. The pins extend out through the skin. A metal rod or bar (fixator) is then attached to the pins outside the body. Fixation keeps the bone in the best position for healing. When the bone has healed enough to hold together, the fixator is removed.
How is external fixation placed?
The surgery to place the fixator is done in the hospital. Here is an overview of what to expect:
Your child will be given general anesthesia. This is medicine that keeps your child free of pain and lets them sleep through the procedure.
The fractured bone ends are moved back into alignment. This is called reduction.
Small incisions are made in the skin on either side of the break. Metal pins or screws are placed into the bone on either side of the break through these incisions.
A bar (fixator) is attached to the pins on the ends that sit outside the body.
Your child may remain in the hospital for a few days after the surgery. Before your child leaves the hospital, you will be shown how to care for your child at home.
If the fractured bone is in the leg, your child may be told not to put their full weight on it. This means crutches or a walker may be used to aid walking.
When is the fixator removed?
Healing of the fracture generally takes a few months. When the surgeon determines that the fracture has healed, the fixator is removed. This is often done as an outpatient surgical procedure.
What are the risks and possible complications of external fixation?
Infection where pins come through the skin (common)
Failure of the bone to heal
Refracture of the bone after the fixator is removed
How do I care for the external fixator?
Follow any instructions you are given for caring for your child.
Don't let your child or your child’s siblings or friends touch or play with the bar or pins.
Clean around the pins carefully. Watch for signs of infection (pain, swelling, redness, pus or white fluid, warmth around the pins, fever, or chills).
When to call the healthcare provider
Call the healthcare provider or get medical care right away if your child has any of these symptoms while the fixator is in place or after it is removed:
Fever (see "Fever and children" below)
Chills
Unusually drowsy or very fussy
A seizure
Warmth, redness, swelling, or oozing of the skin around pins
Increased pain
Tingling or numbness or swelling of the leg
Problems with the fixator
After the fixator is removed, inability to put weight on the injured leg
Any drainage that comes through skin or out of the end of the hardware
Blisters
Decreased ability to move extremity past the hardware
A bad odor from the hardware or skin incision
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The healthcare provider may want to confirm with a rectal temperature.
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
First, ask your child’s healthcare provider how you should take the temperature.
Rectal or forehead: 100.4°F (38°C) or higher
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
Rectal, forehead, or ear: 102°F (38.9°C) or higher
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
Repeated temperature of 104°F (40°C) or higher in a child of any age
Fever of 100.4° (38°C) or higher in baby younger than 3 months
Fever that lasts more than 24 hours in a child under age 2
Fever that lasts for 3 days in a child age 2 or older