When Your Child Has Swimmer’s Ear
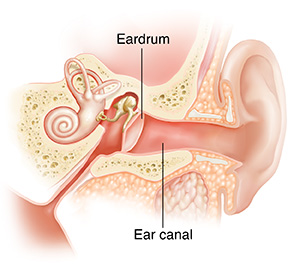
If your child spends a lot of time in the water and is having ear pain, they may have developed swimmer's ear (otitis externa). It's a skin infection that happens in the ear canal, between the opening of the ear and the eardrum. When the ear canal becomes too moist, bacteria or fungus can grow. This causes pain, swelling, and redness in the ear canal.
Who is at risk for swimmer’s ear?
Children are more likely to get swimmer’s ear if they:
-
Swim
-
Lie down in a bathtub
-
Clean their ear canals roughly (this causes tiny cuts or scratches that easily get infected)
-
Have ear canals that are naturally narrow
-
Have excess earwax that traps fluid in the ear canal
What are the symptoms of swimmer’s ear?
The most common symptoms of swimmer’s ear are:
-
Ear pain, especially when pulling on the earlobe or when chewing
-
Redness or swelling in the ear canal or near the ear
-
Itching in the ear
-
Drainage from the ear
-
Feeling like water is in the ear
-
Fever
-
Problems hearing
How is swimmer’s ear diagnosed?
The healthcare provider will examine your child. They will also ask questions to help rule out other causes of ear pain. The healthcare provider will look for:
-
Redness and swelling in the ear canal
-
Drainage from the ear canal
-
Pain when moving the earlobe
How is swimmer’s ear treated?
To treat your child’s ear, the healthcare provider may recommend:
-
Medicines such as antibiotic or antiseptic (acetic acid) ear drops or a pain reliever that is put in the ear. Antibiotic medicine taken by mouth (orally) is not recommended.
-
Over-the-counter pain relievers such as acetaminophen and ibuprofen. Don't give ibuprofen to babies younger than 6 months of age or to children who are dehydrated or constantly vomiting. Don’t give your child aspirin to relieve a fever. Using aspirin to treat a fever in children could cause a serious condition called Reye syndrome.
The provider may also clean out the child's ear.
Don't give your child any other medicine without first asking your child's healthcare provider, especially the first time.
How can you prevent swimmer’s ear?
Ask your child's healthcare provider about using the following to help prevent swimmer’s ear:
-
After your child has been in the water, have your child tilt their head to each side to help any water drain out. You can also dry their ear canal using a blow dryer. Use a low air and cool setting. Hold the dryer at least 12 inches from your child’s head. Wave the dryer slowly back and forth—don’t hold it still. You may also gently pull the earlobe down and slightly backward to allow the air to reach the ear canal.
-
Use a tissue to gently draw water out of the ear. Your child’s healthcare provider can show you how.
-
Use over-the-counter ear drops if the healthcare provider suggests this. These help dry out the inside of your child’s ear. Smaller children may need to lie down on a couch or bed for a short time to keep the drops inside the ear canal.
-
Gently clean your child’s ear canal. Don't use cotton swabs.
When to call your child’s healthcare provider
Call your child's healthcare provider if your child has any of the following:
-
Increased pain, redness, or swelling of the outer ear
-
Ear pain, redness, or swelling that does not go away with treatment
-
Fever (see Fever and children, below)
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
- Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
- Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
- Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
- Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
- Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
- First, ask your child’s healthcare provider how you should take the temperature.
- Rectal or forehead: 100.4°F (38°C) or higher
- Armpit: 99°F (37.2°C) or higher
- A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
- Rectal or forehead: 102°F (38.9°C) or higher
- Ear (only for use over age 6 months): 102°F (38.9°C) or higher
- A fever of ___________ as advised by the provider
In these cases:
- Armpit temperature of 103°F (39.4°C) or higher in a child of any age
- Temperature of 104°F (40°C) or higher in a child of any age
- A fever of ___________ as advised by the provider