Understanding Venous Thromboembolism
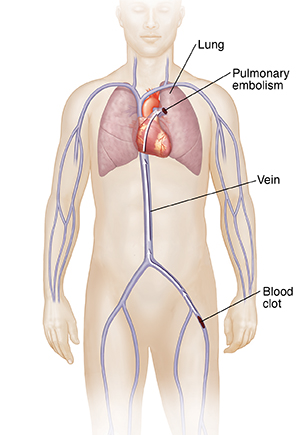
Venous thromboembolism is when a blood clot forms in a vein. The term refers to two linked conditions: deep vein thrombosis (DVT) and pulmonary embolism (PE). If you have DVT, a blood clot has formed in a deep vein. It often happens in a leg. Sometimes this clot can break free and travel to your lungs. Once there, it can block blood flow. This is a PE, which is a health emergency.
How to say it
VEE-nuhs thrawm-boh-EHM-boh-lih-zuhm
What causes venous thromboembolism?
A blood clot can form in a vein for many reasons. The cause may be partly your genes. For example, you may have a protein deficiency or a blood-clotting disorder. Your family history may also make you more prone to the problem.
Other things can also raise your chance for a blood clot in a vein. These include:
-
Major surgery, such as a joint replacement
-
Injury, such as a broken leg or damaged spinal cord
-
Cancer
-
Heart failure
-
Older age
-
Obesity
-
Smoking
-
Some medicines, such as birth control pills or hormone replacement therapy
-
Pregnancy
-
Long periods of not moving enough, such as after a surgery or on a long airline flight
Symptoms of venous thromboembolism
You may have no symptoms. But if you do, they can start quickly. Symptoms of DVT are:
-
Redness near the vein
-
Swelling
-
Pain
-
Changes in the color of the skin
A PE is when the blood clot travels to the lungs. It is a health emergency. It can cause trouble breathing, chest pain, coughing up blood, and an irregular heartbeat. Symptoms may look like those of a heart attack. It can cause sudden death.
Treatment for venous thromboembolism
The goal of treatment is to break up any blood clots and stop new ones from forming. A PE is then less likely to happen. Treatment includes:
-
Blood thinners. These medicines may be given as a shot, through an IV (intravenous), or as a pill. You may need to take them for a few months or longer. It depends on the cause of the blood clot.
-
Walking. Once your symptoms are under control, your healthcare provider may recommend that you walk. You may not be able to walk too far at first, such as after a surgery. But it will stop more blood clots from forming and help you feel better.
-
Compression socks. These socks or other similar devices can lower your risk for blood clots. They gently put pressure on the lower leg. This may help ease pain and swelling.
-
Inferior vena cava filter. This small metal device is put into your inferior vena cava. That’s the main vein that runs from your legs to your heart and lungs. It catches large clots before they reach these organs. It can stop a PE. You may need this treatment if you aren’t able to take blood thinners.
-
Surgery. In some cases, you may need surgery to remove a clot, especially if it has already reached the lungs.
Possible complications of venous thromboembolism
-
New clots
-
High blood pressure in the arteries to the lungs (pulmonary hypertension)
-
Weak valves in a vein (post-thrombotic syndrome), which can cause cramping, pain, and swelling
-
Bleeding
-
Death
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Redness, swelling, or fluid leaking from your incision that gets worse
-
Pain that gets worse
-
Symptoms that don’t get better, or get worse
-
New symptoms