Knee Ligament Repair
What is knee ligament repair or reconstruction?
Ligaments are bands of tough, elastic connective tissue that surround a joint to give support. They also limit the joint's movement.
The knee joint may become unstable when ligaments are damaged. Ligament damage often happens from a sports injury. A torn ligament severely limits correct knee movement. This results in the inability to pivot, turn, or twist the leg. Surgery is a choice to fix a torn ligament if other treatment does not work.
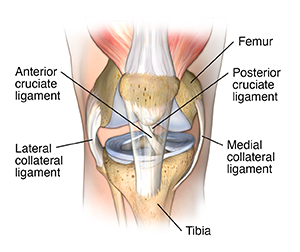
The ligaments in the knee connect the femur (thighbone) to the tibia (shin bone). There are 4 major ligaments in the knee:
- Anterior cruciate ligament (ACL). This controls rotation and forward movement of the tibia (shin bone).
- Posterior cruciate ligament (PCL). This controls backward movement of the tibia (shin bone).
- Medial collateral ligament (MCL). This gives stability to the inner knee.
- Lateral collateral ligament (LCL). This gives stability to the outer knee.
Why might I need a knee ligament repair or reconstruction?
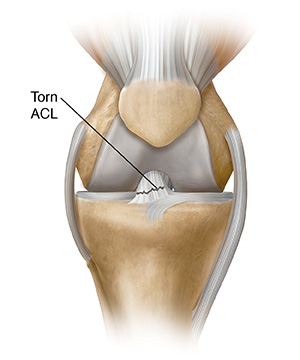
The ACL is toward the front of the knee. It's the most common ligament to be injured. The ACL is often stretched or torn during a sudden twisting motion. For instance, when the feet stay planted one way, but the knees turn the other way. Skiing, basketball, and football are sports that have a higher risk of ACL injuries.
The PCL is toward the back of the knee. It's also a common knee ligament to be injured. But the PCL injury often happens with sudden, direct impact. This can happen in a car accident or during a football tackle.
The MCL is on the inner side of the knee. It's injured more often than the LCL,. This is on the outer side of the knee. Stretch and tear injuries to the collateral ligaments are usually caused by a blow to the side of the knee. This includes when playing hockey or football.
Early medical treatment for knee ligament injury may include:
- Rest
- Ice packs (to reduce swelling that happens within hours of the injury)
- Compression (from an elastic bandage or brace)
- Elevation (keeping it raised)
- Pain relievers
A knee ligament tear may be treated with the following:
- Muscle-strengthening exercises
- Protective knee brace (for use during exercise)
- Limiting activity
Knee ligament repair or reconstruction is a treatment for a tear of a knee ligament that results in instability in the knee. This repair or reconstruction is done by an orthopedic surgeon. This is a surgeon who specializes in treating bone, muscle, joint and tendon problems. People with a torn knee ligament may be unable to do normal activities that require twisting or turning at the knee. The knee may buckle or “give way.” Repair or reconstruction surgery may be an effective treatment if medical treatments don't work well.
The surgery to fix a torn knee ligament with a repair is done by stitching (suturing) the torn ligament. The surgery to correct a torn knee ligament with reconstruction is done by replacing the ligament with a piece of healthy tendon. A tendon from the kneecap or hamstring, for instance, is grafted into place to hold the knee joint together. The tendon graft may come from the person (autograft). Or it may come from an organ donor (allograft).
There may be other reasons for your healthcare provider to advise a knee ligament repair or reconstruction.
What are the risks of knee ligament repair or reconstruction?
As with any surgery, complications can happen. Some possible complications are:
- Bleeding
- Infection
- Blood clots in the legs or lungs
Some people may have pain, limited range of motion in the knee joint, and some swelling in the knee after surgical ligament repair or reconstruction. Others have increased motion in the knee joint as the graft stretches over time.
There may be other risks depending on your specific health condition. Talk about any concerns with your surgeon before the procedure.
How do I get ready for a knee ligament repair or reconstruction?
- Your surgeon will explain the procedure to you. Ask any questions that you might have about the procedure.
- You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
- In addition to a complete health history, your healthcare provider may do a complete physical exam. This is to make sure that you are in good health before having the procedure. You may have blood tests or other diagnostic tests.
- Tell your surgeon if you are sensitive to or are allergic to any medicines, latex, tape, and anesthetic agents (local and general).
- Tell your surgeon about all medicines (prescribed and over-the-counter) that you are taking. This includes vitamins, herbs, and other supplements.
- Tell your surgeon if you have a history of bleeding disorders. Or if you are taking any blood-thinning (anticoagulant) medicines, aspirin, or other medicines that affect blood clotting. You may need to stop these medicines before the procedure.
- Tell your surgeon if you are pregnant or think you could be. .
- Follow all directions you are given for not eating or drinking before your surgery.
- You may receive a sedative before the procedure to help you relax. You will need to arrange for someone to drive you home. This is because the sedative may make you drowsy.
- You may meet with a physical therapist before your surgery to discuss rehabilitation.
- Arrange for someone to help around the house for a week or two after you are discharged from the hospital.
- Your provider may request other specific preparations based on your health condition.
What happens during a knee ligament repair or reconstruction?
Knee ligament repair or reconstruction may be done on an outpatient basis. In rare cases it may be done as part of your stay in a hospital. Procedures may vary depending on your condition and your surgeon's practices.
Knee ligament repair or reconstruction may be done while you are asleep under general anesthesia. Or it may be done while you are awake under spinal anesthesia. You will have no feeling from your waist down if spinal anesthesia is used. Your surgeon will discuss this with you in advance.
Generally, knee ligament repair or reconstruction surgery follows this process:
- You will be asked to remove clothing and will be given a gown to wear.
- An IV (intravenous) line may be started in your arm or hand.
- You will be positioned on the operating table.
- The anesthesiologist will continuously keep track of your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- The skin over the surgical site will be cleansed with an antiseptic solution.
- The surgeon will make several small incisions in the knee area.
- The surgeon will do the surgery using an arthroscope. This is a small tube-shaped tool that is inserted into a joint. The surgeon may reattach the torn ligament or reconstruct the torn ligament by using a part (graft) of the patellar tendon (that connects the kneecap to the tibia), the hamstring tendon (from the back of the thigh), or other autografts. The tendon graft may come from the person (autograft). Or it may come from an organ donor (allograft).
- The surgeon will drill small holes in the tibia and femur where the torn ligament was attached.
- The surgeon will thread the graft through the holes. Then it will be attached with surgical staples, screws, or other means. Over time, bone grows around the graft.
- The incision will be closed with stitches or surgical staples.
- A sterile bandage or dressing will be applied.
What happens after a knee ligament repair or reconstruction?
You will be taken to the recovery room to be watched after the surgery. Your recovery process will vary depending on the type of anesthesia that is given. You will be taken to your hospital room or discharged to your home once your blood pressure, pulse, and breathing are stable and you are alert. Knee ligament repair or reconstruction is often done on an outpatient basis.
You may be given crutches and a knee immobilizer before you go home.
It's important to keep the surgical area clean and dry once you are home. Your healthcare provider will give you specific bathing instructions. The stitches or surgical staples will be removed during a follow-up office visit.
Take a pain reliever for soreness as advised by your surgeon. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only advised medicines.
You may be asked to raise (elevate) your leg and apply an ice bag to the knee several times per day for the first few days to help reduce swelling. Your provider will arrange for an exercise program to help you regain muscle strength, stability, and range of motion. Physical therapy is a key part of recovery.
Tell your surgeon if you have any of the following:
- Fever or chills
- Redness, swelling, bleeding, or other drainage from the incision site
- Increased pain around the incision site
- Numbness or tingling in the leg
- Calf swelling or soreness
You may resume your normal diet unless your provider advises you differently.
It may be hard for a few weeks to resume your normal daily activities because of the limited mobility. You may need someone at home to help you. You should not drive until your provider tells you to. Other activity restrictions may apply. Full recovery from the surgery and rehab may take a few months.
Your surgeon may give you additional or alternate instructions after the procedure, depending on your particular situation.
Next steps
Before you agree to the test or procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how you will get the results
- Who to call after the test or procedure if you have questions or problems
- How much you will have to pay for the test or procedure
Treating ACL Injuries
Treating Anterior Cruciate Ligament (ACL) Injuries
The ACL (anterior cruciate ligament)
is a band of tough, fibrous tissue that stabilizes the knee. Injuries to the ACL are
very
common, especially among athletes. Treatment for your injury may or may not involve
surgery. Treatment depends on the severity of the injury and how active you hope to
be in
the future. Treatment also depends on the type of activities you wish to participate
in.
Your healthcare provider can discuss your treatment options with you.
Reduce pain and swelling
Whether or not you have surgery, you can help reduce pain and swelling with rest, ice, compression, and elevation. Rest with your knee elevated above heart level. Put ice on your knee 3 to 5 times a day for 10 to 15 minutes at a time. Keep a thin cloth between the ice and your skin. A compressive wrap may also help reduce swelling. Take any medicines that are prescribed and follow any other instructions you’re given.
Use crutches
Crutches can help you get around during your recovery. They reduce stress on your knee. Follow your healthcare provider’s advice about the use of crutches and how much weight to put on your injured leg. Use crutches or a brace for as long as advised.
If you need surgery
For severe ACL injuries, you may need a procedure called ACL reconstruction. This is surgery that uses a graft (new tissue) to replace a torn ligament. If surgery is needed, your healthcare provider can give you more information about it.
Rehabilitation
Whether or not you have surgery, rehabilitation exercises are important. Exercise is needed to strengthen the muscles that support your knee. It will also help you regain flexibility, reduce pain, and prevent other knee problems in the future. Your healthcare provider can show you the best exercises for your knee. They will also tell you how long and how often to exercise.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
- Severe or increasing pain in your knee or leg
- Swelling in your entire leg
- Redness or warmth in your leg
- Heat, swelling, or tenderness in your calf
- Fever that lasts more than 24 hours
Treating MCL Problems
Treating Medial Collateral Ligament (MCL) Problems
Treatment for an MCL injury can be nonsurgical or surgical. Nonsurgical treatment is used much more often. With either one, rehab will be part of your treatment.
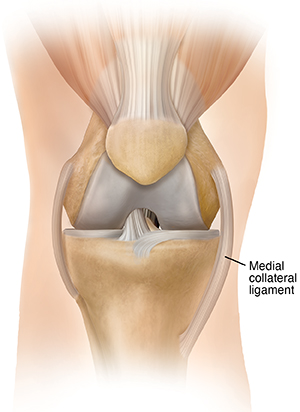
Nonsurgical treatment
This treatment starts with rest, ice, and elevation. This eases pain and swelling. In the next stage, you start exercises to improve your knee’s range of motion, strength, and flexibility. You may need a brace for weeks after your injury. Using crutches or a brace rests your joint, helping it to heal.
Surgery
Surgery is seldom used to fix an MCL injury. But sometimes it is advised, especially if some other part of your knee is hurt. Open surgery is used to screw or stitch the MCL back into place. If fixing the original MCL is not possible, an MCL graft may be used. Based on their location, other knee injuries may be fixed using arthroscopy. With arthroscopy, a tiny camera lets your healthcare provider see inside the joint. Tools are put in through small cuts to fix the joint.
Pre-op checklist
-
Stop taking aspirin and other medicines 7 days before surgery, or as your healthcare provider directs.
-
Arrange to get correctly sized crutches to use as you heal.
-
Don’t eat or drink 10 to 12 hours before surgery (or as your healthcare provider directs).
-
Arrange for someone to drive you home after surgery.
After surgery
Right after surgery, you’ll spend a few hours in a recovery unit. Your knee will be bandaged. Ice will be applied, and your leg raised. Depending on the surgery performed, physical therapy may start shortly after. A brace and crutches are often used after surgery. You may have limits on weight bearing and activity while you heal.