Lung Cancer
The team at Saint Luke’s Cancer Institute has deep experience in treating both early stage and complex cases of lung cancer.
Lung Cancer: Introduction
What is cancer?
Cancer may seem complex. But at its core, cancer is simple. Normal cells grow and die when your body needs them to. Cancer is what happens when certain cells grow even though your body doesn’t need them.
In many cases, these cancerous cells form a lump or mass called a tumor. Since cancerous cells don’t act like normal cells, tumors can prevent your body from working correctly. Given time, they can also spread, or metastasize, to other parts of the body.
Lung cancer is cancer that starts in the cells that make up the lungs. It isn’t cancer that spreads to the lungs from other parts of the body. This is key because treatment is based on the original site of the tumor. For example: If a tumor begins in the breast and spreads to the lungs, it would be treated as metastatic breast cancer—not lung cancer.
Understanding the lungs
The lungs are sponge-like organs in your chest. Their job is to bring oxygen into the body and to get rid of carbon dioxide. When you breathe air in, it goes into your lungs through your windpipe (trachea). The trachea divides into tubes called bronchi, which enter the lungs. These divide into smaller branches called bronchioles. At the end of the bronchioles are tiny air sacs called alveoli. The alveoli move oxygen from the air into your blood. They take carbon dioxide out of the blood. This leaves your body when you breathe out (exhale).
Your right lung is divided into 3 sections (lobes). Your left lung has 2 lobes.
Types of lung cancer
There are two main types of lung cancer: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Understanding the differences between these types may lessen anxiety about your diagnosis and treatment.
Non-small cell lung cancer
NSCLC accounts for 85% to 90% of lung cancer cases. There are 3 main subtypes. Each subtype is named for the type of cell it develops in:
-
Adenocarcinoma. This is the most common type of lung cancer—particularly among the minority of non-smokers who get the disease. It tends to appear on the outer edges of the lungs and grows more slowly than the other subtypes.
-
Squamous cell carcinoma (epidermoid carcinoma). This type of cancer develops more often in smokers or former smokers than lifetime nonsmokers. It tends to start in the center of the lungs near the bronchial tubes.
-
Large cell carcinoma. The least common NSCLC, large cell carcinoma can begin anywhere in the lung. It tends to grow more quickly than the other subtypes, which can make it harder to treat.
Despite minor differences, they are often treated the same way.
Small cell lung cancer
Only about 1 in 10 to 3 in 20 people diagnosed with lung cancer have small-cell lung cancer (also called oat cell cancer). It's also almost exclusively found in smokers. It tends to grow more quickly than NSCLC. It often spreads to other parts of the body at an earlier stage.
How lung cancer spreads
Lung cancer acts differently in different people. But when it spreads, it tends to go to the same places. First: lymph nodes in the center of the chest. It may also spread to lymph nodes in the lower neck.
Lymph nodes are small clusters of immune system cells.
During later stages, lung cancer may spread to more distant parts of the body, such as the liver, brain, or bones.
Talk with your healthcare provider
If you have questions about lung cancer, talk with your healthcare provider. They can help you understand more about this cancer.
Early Detection
Lung Cancer: Early Detection
If lung cancer is detected early, when it’s small and hasn’t had the chance to spread, it is more likely to be treated successfully. Unfortunately, lung cancer can be hard to catch at an early stage. People with lung cancer often don’t show symptoms until it’s more advanced. Even then, it’s easy to attribute those symptoms to other causes.
This is where screening comes in. Simply put, screening is the process of looking for cancer and other diseases in people who don’t have symptoms. If you have a high risk for lung cancer, these tests could save your life.
What is a low-dose CT scan?
Studies have shown that low-dose CT (LDCT) scans can help detect lung cancer early in certain high-risk people. This specifically includes heavy smokers ages 55 to 74.
LDCT scans use X-rays to create detailed 3-D images of your lungs. They are totally painless and require no special preparation. All you do is lie down on a narrow table as it passes through a ring-shaped CT scanner. At most, you may be asked to hold your breath a few times during the test.
LDCT scans can spot abnormal areas that regular chest X-rays might miss. The benefit is significant: a lower risk of dying from lung cancer. Some potential downsides, however, include:
- Many abnormalities surfaced in LDCT scans do not turn out to be cancer. These findings can cause unnecessary anxiety.
- More tests may determine whether the abnormal area is cancer. Sometimes, these exams can lead to complications.
- Each scan uses a small amount of radiation.
Keep in mind: LDCT scans do not find all lung cancers. It’s also possible the cancers they do find may have already progressed to a later stage.
Who should get screened for lung cancer?
The U.S. Preventive Services Task Force (USPSTF) and other expert groups have created specific guidelines for who should get screened. They recommend yearly LDCT scans for people who are:
- Between the ages of 50 and 80 AND
- Current smokers, or former smokers who have quit in the past 15 years AND
- Have a 20-pack year history of smoking. A pack-year is the equivalent of smoking an average of one pack of cigarettes per day for a year. In other words, smoking a pack a day for 20 years equals 20 pack-years. Smoking two packs a day for 10 years also equals 20 pack-years.
The USPSTF says that screening can stop once a person has not smoked for 15 years or has a health problem that limits their life expectancy or their ability to have lung surgery.
Questions to ask your healthcare provider
Even if you meet all the testing criteria, it’s important to talk with your healthcare provider about your personal health and risk. Some questions to consider asking are:
-
What are the limits and risks of screening? Understanding potential outcomes before you go for a screening may reduce feelings of fear or anxiety.
-
Am I healthy enough to get a screening? The risks of screening outweigh the benefits for certain people. For example, if someone can’t have lung surgery to remove the cancer, screening may not be a good option.
-
Where should I go for a lung cancer screening and treatment, if needed? Expert groups advise to have lung cancer screenings at centers with the proper experience. These facilities should have specialists on staff. They can handle follow-up appointments, questions, and care.
-
Is there any cost associated with the annual screening? Medicare and many private health insurance plans cover lung cancers screenings. It’s a good idea to ask your healthcare provider whether insurance will cover it before scheduling a test.
Diagnosis
Lung Cancer: Diagnosis
How is lung cancer diagnosed?
If your healthcare provider thinks you may have lung cancer, you will need certain exams and tests to be sure. Diagnosing lung cancer starts with your healthcare provider asking you questions. You'll be asked about your health history, your symptoms, possible risk factors, and family history of disease. A physical exam will be done. You might need to:
-
Have a sputum cytology test . Each morning for 3 to 5 days in a row, you'll collect the mucus (sputum) that you cough up from your lungs. It's then sent to a lab and looked atunder a microscope to see if there are cancer cells in it.
-
Have blood drawn. A needle might be used to take a small amount of blood from your hand or arm. Blood tests can show how well certain organs are working and give an idea of your overall health.
-
Get a chest X-ray. This is done to look for changes in your lungs, like tumors or fluid buildup.
-
Schedule other imaging tests. These are done to get a better picture of your lungs. A CT scan gives detailed X-ray pictures of the inside of your body and is most often used.
Any of these tests might suggest that you have lung cancer. If imaging tests show something that doesn't look normal, such as a mass or fluid, you'll need to have a biopsy. This is when a healthcare provider takes out a tiny sample of the mass or some of the fluid for testing at a lab. A biopsy is almost always needed to diagnose lung cancer.
What kind of biopsy might I need?
The way a biopsy sample is taken out depends partly on where the tumor is and how big it is. Your healthcare provider may suggest one or more of the tests below to help do a biopsy and diagnose lung cancer.
After any kind of biopsy, the tissue samples are sent to a lab. They're looked at under a microscope and tested for cancer cells. It often takes up to a week for biopsy results to come back. Along with telling if you have lung cancer, a biopsy can often tell exactly what kind of lung cancer it is.
A lung biopsy can be done in many ways:
-
Bronchoscopy
-
Needle biopsy
-
Thoracentesis
-
Thoracotomy or thoracoscopy
Each is briefly described below. Your healthcare provider can give you more details on the kind of biopsy you're going to have.
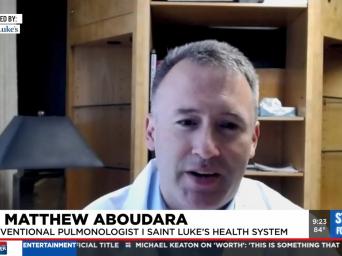
Bronchoscopy
A pulmonologist often does this test. This healthcare provider specializes in lung diseases. The pulmonologist uses a long, thin, lighted tube called a bronchoscope to get a sample in this type of biopsy. The bronchoscope may be flexible or rigid. It's put in through your mouth or nose, through your breathing passages, and into your lungs. It has a tiny camera on the end so that your healthcare provider can see inside your lungs to get the sample from the right place.
How it is done
This procedure often takes about an hour. If your healthcare provider is using a flexible bronchoscope, a numbing medicine (local anesthesia) is sprayed inside your nose or mouth. You may feel like fluid is running down your throat. It might make you cough or gag. This stops when the numbness kicks in. You may also have an IV (intravenous) line put into a vein in your hand or arm. It's used to give you medicine to help you relax. If your healthcare provider uses a rigid bronchoscope, you'll get general anesthesia through an IV. This means medicines are used so you sleep and don't feel pain during the test.
With either type of bronchoscopy, the healthcare provider might put a small amount of saltwater (saline) into your lung passageways. This liquid flushes the area and helps collect cells, fluids, and other materials in your airways. The collected material is then taken out through the bronchoscope and sent for testing. Your healthcare provider may also put tiny brushes, needles, or forceps (which are like tweezers) through the bronchoscope to collect cells from any suspicious-looking tissue. All the collected samples are sent to a lab and checked for cancer. Sometimes the provider will examine lymph nodes or take a biopsy using ultrasound imaging to guide the bronchoscopy. This is called an endobronchial ultrasound. An ultrasound uses sound waves to create an image.
As the numbing medicine wears off, your throat may feel scratchy. You won’t be able to eat for a few hours. You'll need to have someone drive you home. Some people want to rest the day after the biopsy. So you may want to take the day off from your normal activities.
Needle biopsy
This is also called needle aspiration or transthoracic needle aspiration. Your healthcare provider may use this test if the tumor can’t be reached with a bronchoscope. To do it, a thin, hollow needle is put through the skin of your chest and into the tumor to remove some tissue. Often an X-ray, ultrasound, or CT scan is done at the same time. This helps the healthcare provider see the tumor and guide the needle into it.
How it is done
A needle biopsy is often done by a healthcare provider called an interventional radiologist. An imaging scan is often used to help your healthcare provider see exactly where to get the cells that might be cancer. You might sit with your arms resting on a table or lie down. It depends on where the tumor is and the kind of imaging test used. Either way, it’s important that you don’t move.
You may get medicine to relax you and help you stay still. The healthcare provider uses a small needle to put numbing medicine in your skin. A tiny cut might be made in your skin to get the bigger biopsy needle in. You might feel pressure and a short, sharp pain when the needle touches your lung. The needle is then put into the tumor or abnormal tissue and a syringe is used to pull out cells. The needle is then taken out and pressure is put on the site until the bleeding stops. It's then covered with a bandage.
The healthcare provider sends the collected cells to a lab to be tested for cancer cells. Right after the biopsy, you'll get a chest X-ray. This is to make sure there are no problems, like a collapsed lung (pneumothorax). You may be able to drive yourself home after the test if you were not given any medicines that cause drowsiness. But ask before the test is done to be sure this is OK.
Thoracentesis
This is also called a pleural fluid aspiration or a pleural tap. It might be done if fluid has built up around your lungs. It's used to see if the fluid contains cancer cells. A healthcare provider puts a thin, hollow needle through your skin to drain out the fluid. This test may be done to diagnose lung cancer. It's also used to drain fluid that's making it hard for you to breathe.
How it is done
You will lie on a bed or sit on the edge of a bed or a chair and rest your head and arms on a table. A small needle is used to put numbing medicine into the skin over the part of your lung that has fluid in it. Then the healthcare provider puts in the thoracentesis needle. It goes in above a rib and into the space between the lining of the outside of your lungs and your chest wall (called the pleural space). You may feel pressure. The fluid then drains out or is pulled into a syringe. It's sent to a lab to be checked for cancer. Ask your healthcare provider if you'll be able to drive yourself home after this test.
Thoracotomy or thoracoscopy
Thoracotomy and thoracoscopy are types of surgery done in an operating room. The surgeon opens up your chest to look for lung cancer. This is often done when the healthcare provider can’t make a clear diagnosis using any of the other methods. If possible, the surgeon takes out the entire tumor.
How it is done
You must be in the hospital for a thoracotomy. An IV (intravenous) line is put into a vein in your hand or arm. It's used to give you medicine that makes you sleep and not feel pain during the surgery. The surgeon cuts between your ribs to reach your lungs and look for diseased tissue. Some or all of the diseased tissue is taken out and sent to a lab to be checked for cancer. When you wake up, you'll have a tube in your chest to drain air, fluid, and blood. You may need to stay in the hospital for a couple of days. During that time, you will get pain medicine as needed.
A thoracoscopy is much the same, but smaller cuts are used. It might be done to look atand take a biopsy from the outer surface or the linings of the lungs and other nearby structures. Like a thoracotomy, you get medicine so that you sleep during the surgery. But instead of making one long cut, the surgeon makes a few small cuts in the chest wall. A long, thin tool with a small camera on the end is put in through one of the cuts so the surgeon can see inside your body. Long, thin tools are then put in through the other cuts to take out samples of any diseased tissue. Because the cuts are smaller, people often recover more quickly from this type of procedure.
Getting your test results
Ask your healthcare provider how long it will take to get your test results and how you'll get them. Will it be a phone call? Do you need to set up an appointment?
If lung cancer is found, your provider will talk with you about other tests you may need. Make sure you understand the results and what your next steps should be.