Vascular Hemodialysis Access
At Saint Luke’s Hospital, we provide a multidisciplinary approach to managing your dialysis access needs. Our surgeons work closely with nephrology and are available to evaluate an existing dialysis access that may be causing you problems, such as pain, discomfort, or visible aneurysm formation.
We also work with a team of interventional radiologists to troubleshoot more immediate problems that are causing a delay in your hemodialysis treatments.
For more information, call our vascular access coordinator at 816-932-8311.
Creating a Hemodialysis Access
Before hemodialysis can be done, a way for blood to leave and return to your body (an access) is needed. During hemodialysis, needles placed into the access carry blood to and from the dialyzer. A hemodialysis access is often made in your arm. The 2 main types of accesses are an arteriovenous fistula (AV fistula) and an arteriovenous graft (AV graft). An interdisciplinary team, usually composed of experienced nurses, nephrologists, radiologists, and vascular surgeons, works with the patient to determine the best type of access.
Making your access
The hemodialysis access provides a large volume of fast flowing blood. It involves surgery under anesthesia. You may be able to go home the same day. It is made during a short procedure using 1 of these methods:
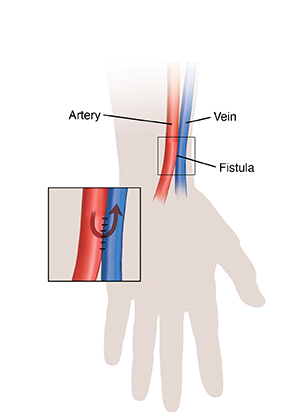
A fistula is made by linking an artery to a nearby vein. The high pressure and blood flow in the artery are transferred into the vein. They help the vein grow in size and thickness. The enlarged vein (fistula) eventually has high blood flow. It becomes thick enough for needles to be placed safely several times each week during hemodialysis. It may need weeks or months to develop before it's ready to be used. A fistula works better than a graft. It also has fewer long-term problems. It is generally the preferred form of access.
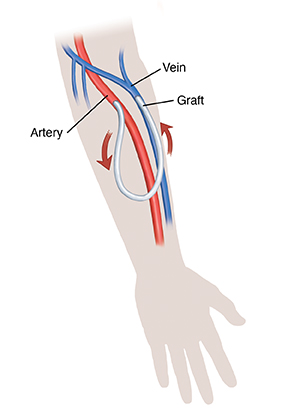
A graft (piece of synthetic tube) may be sewn between an artery and a vein. It's often used if a fistula is not possible because of the small size of your veins. Blood flows quickly through the graft from the artery to the vein. A graft is often ready to use in a few weeks. Needles can be placed into the plastic tube to get blood during dialysis.
Both types of access may take weeks to months before they can be used. If dialysis is needed right away, a short-term venous catheter is used. A catheter that allows two-way blood flow is placed into a large vein. The dialysis tubing is then connected to the catheter. If both the AV fistula and graft don't work, a more permanent venous catheter is used.
The most common complications for hemodialysis access are:
Infection
Clotting
Decreased blood flow from clotting or other narrowing
Caring for Your Hemodialysis Access
It's important to care for and protect your access to help it last. A problem such as an infection or a blood clot may make your access unusable. This may happen more often with an arteriovenous graft than with an arteriovenous fistula. If this occurs, you may need a new access. Follow these guidelines to help protect your access.
Watching for problems
Call your healthcare provider right away if you:
Can’t feel the blood flowing in the access (this sensation is called a thrill)
Have pain or numbness in your hand or arm
Have bleeding, redness, a bluish color, or warmth around your access
Notice your access suddenly bulging out more than usual (a slight bulge is normal)
Have a fever of 100.4°F (38°C) or higher, or as advised by your provider
Follow these and any other guidelines you’re given
Wash your hands often.
Do not wear tight clothes or jewelry around your access.
Do not sleep on your access area.
Do not let anyone take your blood pressure on or draw blood from the arm with the access. Also don’t let anyone put IV (intravenous) lines into it.
Do not get the area wet. Ask your nurse or doctor how to protect the area around the catheter incision and about using a special protective cover when you shower.
Protect your access from being scratched, hit,or cut.
Do not carry anything heavy or do anything that would put pressure on the access.
Check the area every day for signs of an infection such as redness, pain, and swelling. If you have any of these symptoms, a fever or flu-like symptoms call your doctor right away.
Keep the access area clean.
Shower only after your AV fistula or AV graft has completely healed
Wash the access area every day with antibacterial soap and water or as advised by your provider
Change the dressing as often as your doctor tells you to. Always keep the dressing clean and dry. Make sure you have plenty of dressing supplies at home in case you need to change it.
Feeling for your thrill
If you put your fingers over your access, you should feel the blood rushing through it. This is called a thrill, and it feels like a vibration. Feel for the thrill as often as you're told, usually once or twice a day. If you can't feel it, tell your healthcare provider right away. Blood may not be flowing through your access the way it should.
Important numbers
Write the names and numbers of your healthcare providers below or have them programmed into your cellphone,.that way you will know how to get in touch with them.
Healthcare Provider:
Name ___________________ Phone ___________________
Surgeon:
Name ___________________ Phone ___________________
Dialysis Center:
Name ___________________ Phone ___________________
How daily issues affect your health
Many things in your daily life impact your health. This can include transportation, money problems, housing, access to food, and child care. If you can’t get to medical appointments, you may not receive the care you need. When money is tight, it may be difficult to pay for medicines. And living far from a grocery store can make it hard to buy healthy food.
If you have concerns in any of these or other areas, talk with your healthcare team. They may know of local resources to assist you. Or they may have a staff person who can help.