Push Enteroscopy
Push enteroscopy is a procedure that helps find and treat problems most commonly in your upper to middle small intestine. It’s done using a long, narrow, flexible tube called an enteroscope. There are several types of enteroscopes. The tube has a tiny light and a camera on its tip. It connects through a video feed to a screen where the picture is seen in high definition. This lets your healthcare provider see inside your intestine.
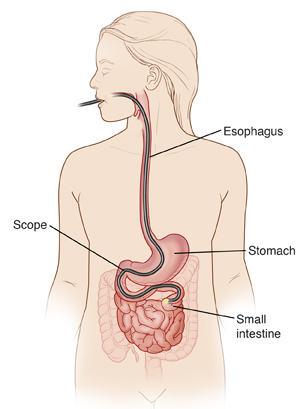
The tube is passed through your mouth. It's then guided through your food pipe (esophagus) and stomach to your small intestine. If needed, a tissue sample (biopsy) may be taken. Some problems can also be treated during the procedure.
More recently, there is a special type of enteroscope to see the lower part of the small intestine. It can be passed through the rectum to get to the lower small bowel. Sometimes these enteroscopes use balloons to help guide the scope as far as it needs to go.
Getting ready for your procedure
Tell your healthcare provider about all the medicines you are taking. This includes all prescription and over-the-counter medicines, vitamins, herbs, and other supplements. It also includes illegal drugs. You may need to stop taking all or some of these medicines before the test.
Follow any directions you’re given for not eating or drinking before the procedure. If you are having an enteroscopy through the rectum, you will be given instructions on a clear liquid diet the day before, and a laxative preparation that evening.
The day of your procedure
The procedure often takes about 25 to 45 minutes. Some procedures may take longer. You will go home the same day.
Before the procedure begins
You will be given medicine to help you relax or sleep (sedation). This is given through an intravenous (IV) line placed in a vein in your arm or hand. Your throat may be numbed with a spray or liquid. You will be given a small plastic guard to protect your teeth. You will be given oxygen to breathe through 2 soft prongs (called a cannula) that sit just inside your nose. You will be connected to a machine to watch your heartbeat.
During the procedure
-
You will lie on your left side. The tube is placed in your mouth, and it moves down your throat. Air is used to expand your gastrointestinal (GI) tract so the lining can be seen more clearly.
-
The tube is guided down your esophagus. It then goes through your stomach and into your small intestine. Your position may be changed, or your healthcare provider may apply pressure over your belly (abdomen), if needed.
-
The tube sends pictures of the GI tract to a screen. The esophagus, stomach, and small intestine are checked.
-
Problems such as bleeding, redness or swelling (inflammation), or growths may be seen. Using tools inserted through the tube, small tissue samples can be taken. These are called biopsies. In some cases, small growths can be removed. Other treatments, such as those to stop bleeding, may be done.
-
The tube is then removed.
After the procedure
Your healthcare provider will talk with you afterward about the results. You’ll rest until you are recovered and can safely go home. Have an adult family member or friend drive you. Plan to rest for the remainder of the day.
Recovering at home
You’ll likely feel sleepy after the test. A mild sore throat, mild gas, and bloating are normal. Once home, follow any instructions you have been given. If you were given medicine to help you relax or sleep, don't drive, operate machinery, or make major decisions until the next day.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Shaking chills
-
Chest pain
-
Black, tarry stool or bloody stool
-
Severe belly pain that doesn't go away when you pass gas
-
Sore throat that doesn’t go away
-
Trouble swallowing
-
Vomiting, especially with blood
-
Any other signs or symptoms indicated by your provider
Follow-up
If you had a biopsy, the results will be ready in about 7 days. Your healthcare provider will talk with you about any further testing or treatment that is needed.
Risks and possible complications
All procedures have some risk. Possible risks of this procedure include:
-
Sore throat or hoarseness
-
Bloating
-
Nausea
-
Allergic reaction to the sedative or numbing medicine
-
Bleeding during or after the procedure
-
Too much bleeding from the biopsy site (if a biopsy is done)
-
A hole or tear (perforation) in the lining of the digestive tract
-
Inhaling food or fluid into the lungs (aspiration)
-
Irregular heartbeat or cardiac arrest. You are at higher risk for this if you have heart or lung disease.