Transoral Resection for Oral Cancer
Transoral resection is surgery to help control or cure oral cancer. It may be a choice if the cancer is small and has not spread. You may hear this surgery called TORS, or transoral robotic surgery. TORS means the healthcare provider is using small robotic tools to do the surgery. If lasers are used, it might be called transoral laser microsurgery (TLM). TORS and TLM need a surgeon to have special skills and experience.
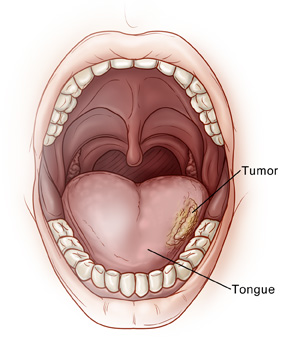
During transoral resection, the tumor is removed through the mouth. The tumor could be on the tongue, under the tongue, inside the cheek, or any place inside the mouth that's fairly easy to reach. Some healthy tissue around the tumor is also removed (margin), to help make sure that no cancer cells remain. This sheet explains transoral resection and what to expect. After surgery, more cancer treatment may be needed, such as chemotherapy and radiation. Your healthcare provider will discuss your treatment plan with you.
Getting ready for surgery
Get ready for the procedure as you have been instructed. Be sure to tell your healthcare provider about all medicines you take. This includes over-the-counter medicines, street drugs, and marijuana. It also includes herbs, vitamins, CBD, and other supplements. You may need to stop taking some or all of them before surgery. Follow any directions you’re given about not eating or drinking before surgery.
Before the surgery
How long the surgery takes depends on how extensive it is. Ask your healthcare team how long you can expect the surgery to last. Before the surgery begins:
-
An IV (intravenous) line is put into a vein in your arm or hand. It's used to give you fluids and medicines.
-
You will be given general anesthesia. This medicine puts you into a deep sleep-like state during the surgery so you don't feel pain.
During the surgery
Here is what to expect during surgery:
-
An endoscope is put into your mouth. This is a thin flexible tube with a light and camera on the end. Your healthcare provider will use it to get a close-up look at the tumor and the healthy tissue around it.
-
Small cuts (incisions) are made and the tumor is removed.
-
Some healthy tissue around the tumor is also removed. This is sent to a lab, where it’s checked for cancer cells.
-
The cut pieces of tissue are joined together with stitches (sutures). These dissolve on their own over time. In some cases, a small skin graft may be needed to help fill in the area that was removed. The graft is stitched in place with sutures.
-
Depending on where the tumor is, you may need a tracheostomy (trach) tube to help you breathe, or a feeding tube to help you eat. If either or both of these are needed, they will be put in at the end of the surgery. These may be needed for just a short time, as you heal. Or they may be permanent. Your healthcare provider will talk with you about this while planning the surgery so you'll know what to expect.
After the surgery
You will be taken to a recovery room to wake up from the anesthesia. You may feel sleepy and nauseated right after surgery. You'll be given pain medicine. Let your healthcare providers know if your pain is not controlled. When you're ready, you will be taken to a hospital room and will likely stay for a few nights.
When it’s time for you to be released from the hospital, have an adult family member or friend ready to drive you. Have someone stay with you for a few days to help care for you as you heal. If you have a trach or feeding tube, you will be shown how to care for these before you go home.
Recovering at home
Once at home, follow the instructions you have been given. Be aware that the surgery may affect your ability to swallow and to speak. You may be referred to a speech therapist. They can help you with these skills starting soon after surgery. During your recovery:
-
Take all antibiotics and pain medicine as directed. Be sure you know how and when to take your medicines, what they're for, and what side effects you should watch for.
-
You may have diarrhea from diet changes, stress, or an infection. Talk with a dietitian about what you can eat to reduce the chances of getting diarrhea.
-
You may have constipation from using opioid pain medicine, from not moving much, or from not eating and drinking as much. Talk with your healthcare provider or nurse about what you can do to prevent constipation.
-
Resume your normal diet slowly as directed by your healthcare provider. To protect your healing mouth, do not eat spicy or acidic foods, such as hot peppers, oranges, and tomatoes. Also don't eat sharp, hard foods like crackers, nuts, and chips. Smooth soups, puddings, milkshakes, and blended fruit drinks will be easiest on your mouth as you heal.
-
Return to your normal daily routine when your healthcare provider says it’s OK. This includes work and exercise.
-
Don't drive until you are no longer taking pain medicines that make you drowsy.
When to call your healthcare provider
Be sure you have a contact number for your healthcare provider. Ask how to get help after office hours and on weekends and holidays. After you go home, call if you have any of these:
-
Chest pain or trouble breathing (call 911)
-
Fever of 100.4° F ( 38° C) or higher, or as directed by your healthcare provider
-
Pain that gets worse or is not relieved by pain medicines
-
Bleeding in your mouth
-
Excessive swelling
-
Choking on food or liquids
-
Severe nausea or vomiting
-
Pain, swelling, or warmth in an arm or leg
Follow-up
During follow-up visits, your healthcare provider will check on your healing. They will talk with you about treatment with radiation or chemotherapy, if needed. Regular checkups are very important. These help to make sure that the cancer has not returned. Regular dental exams may be needed. If you smoke, talk to your healthcare provider about quitting. Smoking makes oral cancer treatment less effective. And it increases your risk for another tumor.
Risks and possible complications
Risks of transoral resection include:
-
Bleeding
-
Blocked airway
-
Blood clots
-
Infection
-
Changes in taste
-
Weight loss
-
Trouble swallowing or speaking after healing (if part of the tongue is removed)
-
Nerve injury, causing numbness of the lip or tongue (may be temporary or permanent)
-
Breathing in (aspirating) food or liquids
-
Risks of anesthesia. The anesthesiologist will talk with you about these.
-
The cancer returns
- Changes in how you look or how your body works