Understanding Subscapular Bursitis
A bursa is a thin, slippery, saclike film that contains a small amount of fluid. A bursa is often found in and around joints. It cushions and protects bones and soft tissues, and stops them from rubbing against each other. If a bursa becomes inflamed and irritated, it's known as bursitis.
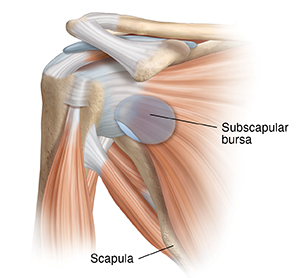
The subscapularis muscle is a large muscle across the front of the shoulder blade. The subscapular bursa is found between the subscapularis muscle and the chest wall. Inflammation of this bursa is called subscapular bursitis.
Causes of subscapular bursitis
These may include:
-
Overuse of the shoulder from things like reaching, lifting, and throwing
-
Injury from a fall or other accident
-
Having rheumatoid arthritis or other types of inflammatory arthritis
Symptoms of subscapular bursitis
The shoulder may be painful or aching. This pain may be worse when raising your arm or lying on the affected shoulder.
Treatment for subscapular bursitis
These may include:
-
Resting your shoulder. This allows the bursa to heal.
-
Prescription or over-the-counter medicines. These can help reduce inflammation, pain, and swelling. NSAIDs (nonsteroidal anti-inflammatory drugs) are the most commonly used medicines. Medicines may be prescribed or bought over the counter. They may be given as pills. Or they may be put on the skin as a gel, cream, or patch.
-
Cold packs or heat packs. These can help reduce pain and swelling.
-
Exercises. These improve shoulder flexibility and strength.
-
Physical therapy. This may include exercises, education, and other treatments.
-
Injections of medicine into the bursa. This may help reduce inflammation and relieve symptoms. This usually is an anti-inflammatory medicine called a corticosteroid.
Possible complications
If your shoulder isn’t given time to heal, symptoms may return or get worse. Also, the problem may become long-term (chronic). This can lead to trouble moving the shoulder joint.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as directed by your provider
-
Chills
-
Symptoms that don’t get better with treatment, or get worse
-
New symptoms