When Your Child Has a Forearm Fracture
Your child has a forearm fracture. That means they have a crack or break in one or both of the forearm bones. The forearm is made up of 2 bones:
Radius. The bone on the thumb side of the forearm.
Ulna. The bone on the little-finger side of the forearm.
Your child may see an orthopedist for evaluation and treatment. An orthopedist is a healthcare provider who diagnoses and treats bone and joint problems.
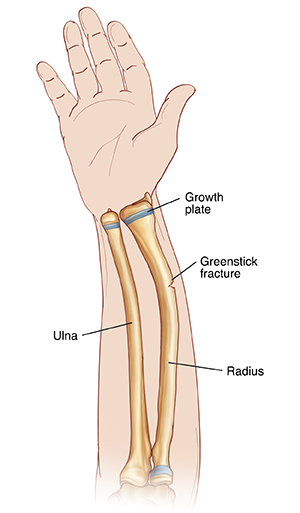
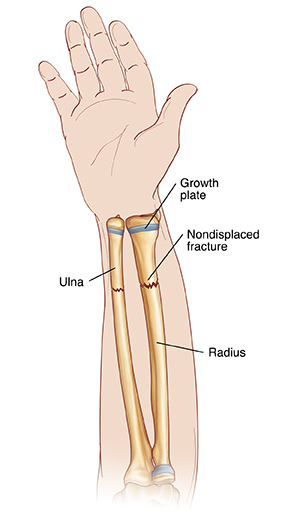
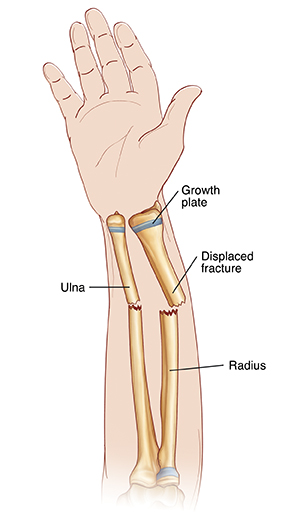
Types of fractures
Bones can break in many ways. Common types of fractures in children are:
Greenstick. The bone bends but doesn’t break all the way through.
Nondisplaced. The bone breaks completely, but the ends remain lined up.
Displaced. The pieces of broken bone are not lined up.
Growth plate. This is a break near or through the growth plate, the soft part of a bone where the bone grows as the child grows. A growth plate injury can slow growth in that bone. Growth plate injuries may be difficult to treat.
Fractures can be open where the broken bone comes through the skin. These may also be referred to as compound fractures. Fractures can also be closed (the broken bone doesn't come through the skin).
What causes forearm fractures?
Forearm fractures can happen when 1 or both of the forearm bones (the radius and ulna) are injured. Falling on an outstretched hand often leads to a forearm fracture. A direct hit to the forearm can also cause a fracture.
What are the symptoms of forearm fractures?
Swelling
Pain
Skin bruising or color change
Extreme pain while putting weight or pressure on the forearm
Crooked appearance
Popping or snapping heard during the injury
Unable to move the arm normally
How are forearm fractures diagnosed?
You may have brought your child to the emergency room for the initial treatment of the forearm fracture. A treatment plan must now be made to make sure the forearm heals correctly. The healthcare provider will ask about your child’s health history and examine your child. An imaging test, such as an X-ray, will be done. Imaging tests show areas inside the body, such as the bones. They give the healthcare provider more information about your child’s injury.
How are forearm fractures treated?
Your child’s treatment plan is determined by the type, location, and severity of the fracture. As instructed, your child should:
Ice the area
3 to 4 times a day for15 to 20 minutes at a time. This can help relieve pain and swelling. To make a cold pack, put ice cubes in a plastic bag that seals at the top. Wrap the bag in a clean towel or cloth. Never put ice or an ice pack directly on the skin. The cold pack can be put right on a cast or splint.Wear a splint (device that keeps the forearm still so it can heal) as instructed while the swelling begins to go down.
Wear a cast for
3 to 6 weeks or more depending on the injury.Elevate the arm to reduce pain and swelling. Keep the forearm above heart level as often as possible.
Some fractures may need closed reduction (moving broken pieces of bone back into alignment). Closed reduction manipulates the bones from outside of the body and needs no incisions. For fractures of the joint, of the growth plate, or severe fractures, open surgery may be necessary. During surgery, fixation devices (pins, plates, or screws) may be put into the broken bone to hold it in place while it heals. These devices may need to be taken out by the healthcare provider
When to call the healthcare provider
Call the healthcare provider or get medical care right away if you child has any of these:
Fever (see “Fever and children” below)
Chills
Tingling, numbness, or pain around the cast or splint
Increasing swelling around the injured area
Increasing pain
Fingers that change color or feel cold
Severe itching under a cast (mild itching is normal)
A cast or splint that feels too tight or too loose
Decreased ability to move fingers
Any drainage that comes through or out of the end of the cast
Blisters
A bad odor that comes from underneath the cast
What are the long-term concerns?
Your child’s forearm may look different than it did before the fracture. It may look slightly crooked. This is normal. The bone is going through a process called remodeling. During remodeling, the repaired bone slowly reshapes itself. The forearm will usually straighten as the bone reshapes. This process often takes
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
Rectal. For children younger than 3 months, a rectal temperature is the most accurate.
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The healthcare provider may want to confirm with a rectal temperature.
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
First, ask your child’s healthcare provider how you should take the temperature.
Rectal or forehead: 100.4°F (38°C) or higher
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
Rectal, forehead, or ear: 102°F (38.9°C) or higher
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
Repeated temperature of 104°F (40°C) or higher in a child of any age
Fever of 100.4° (38°C) or higher in baby younger than 3 months
Fever that lasts more than 24 hours in a child under age 2
Fever that lasts for 3 days in a child age 2 or older