Whipple Procedure
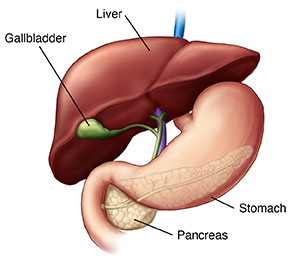
This surgery is also called pancreaticoduodenectomy. It's used to treat cancer of the pancreas. The pancreas is a gland attached to the small intestine. The pancreas makes digestive enzymes and sends them into the intestine to help digest food. It also makes insulin, a hormone that deals with the body’s sugar level. During the surgery, parts of the pancreas, small intestine, and other organs are removed.
The surgery is most often done to treat cancer near the head of the pancreas. It's usually only done if the cancer hasn't spread to other parts of the body (metastasized). But it may also be done to relieve or prevent symptoms (palliation). The procedure may also be done to help cure painful chronic pancreatitis that doesn't respond to other treatments.
The surgery takes at least 5 hours. You'll likely need to stay in the hospital for 1 to 2 weeks afterward.
Before the surgery
Your healthcare provider may have you follow a special, clear liquid diet for 1 to 2 days before the surgery. Also, you’ll have to stop taking medicines such as blood thinners and aspirin. You may be instructed to take a laxative as well.
During the surgery
A needle is placed in a vein in your hand or arm. It’s attached to a tube called an IV line. The IV line gives you fluids. It’s also used to give medicine to prevent pain. This may include a sedative or anesthesia. Depending on the medicine used, you may be drowsy or asleep during the surgery. You may also be given medicine into your back that numbs you from the waist down.
The surgeon will make a cut in your belly (abdomen). If the surgery is for cancer, the surgeon may look at your pancreas and abdomen. This is to make sure that the size and location of the cancerous tumor are as expected. The surgery will only continue if the tumor can be removed safely. The surgeon may also continue the surgery if they feel that it can relieve or prevent your symptoms.
If the surgery proceeds, the head of the pancreas is removed. In some cases, the body of the pancreas is also removed. In addition, a section of the small intestine, the gallbladder, and part of the common bile duct are removed. In some cases, part of the stomach is removed. Finally, nearby lymph nodes are removed.
The remainder of the pancreas and the common bile duct are connected to the intestine. The intestine is then reconnected to the stomach. This restores the pathway for food from the stomach to the remainder of the small intestine, and then to the large intestine.
When the surgery is done, the surgeon closes the incision with sutures or staples. You will have tubes in your incisions called drains. These are usually in place for a few days. You may also have a tube in your nose that goes to your stomach. This drains fluid for a few days. You may also have a tube in your bladder that will drain the urine for a few days.
After the surgery
You’ll be taken to the post-anesthesia care unit (PACU) or intensive care unit (ICU). Nurses will closely watch your condition. You’ll be moved to a hospital room when you’re stable. Medicines will be given to help manage pain and relieve symptoms. When you are able, you will be encouraged to get up and walk. This helps prevent lung and blood flow problems. You won’t be able to eat for a few days. You’ll receive nutrition through your IV. Several days after surgery, you will start on a liquid diet. You will then slowly return to your normal diet. Before you go home, make sure you have all the prescriptions and home care instructions you will need.
Risks and possible complications
All surgeries have risks. The risks of this procedure include:
-
Infection
-
Bleeding
-
Pain
-
Leakage of the connection between the intestine and the bile duct, pancreas, or stomach
-
Surgery fails to resolve the problem
-
Small possibility of developing diabetes, or if you have diabetes, it can become worse
- Developing chronic diarrhea from loss of digestive hormones
- Leg swelling or blood clots
-
Death
- Complications from anesthesia
Recovering at home
Once at home, follow all instructions from your healthcare provider. Make sure to:
-
Take all medicines as directed. Take pain medicines on time. Don’t wait until pain is bad to take them.
-
Care for your incision as instructed. This includes keeping the incision clean and dry, especially when bathing or showering. Don't take tub baths until your healthcare provider says it's OK.
-
Don't lift anything heavy or do strenuous activities, as directed.
-
Walk at least a few times daily. Slowly increase your pace and distance, as you feel able.
-
Don't drive until your provider says it's OK and you're not taking pain medicines.
-
Keep in mind that recovery from major surgery takes time. You will have good days and bad days. Don’t push yourself too hard.
Follow-up
Keep all follow-up appointments with your healthcare provider. If you had cancer, your healthcare provider will discuss any other treatments you need. You may need to take supplements that contain pancreatic enzymes for a time after the surgery.
When to call the healthcare provider
Call the healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Chills
-
Increased redness, pain, swelling, bleeding, or drainage from any incisions
-
Vomiting
-
Excessive bloating
-
Lack of bowel movements
-
Oily, loose stools
-
Jaundice
Call 911
Call 911 right away if you have any of these:
- Trouble breathing
- Chest pain