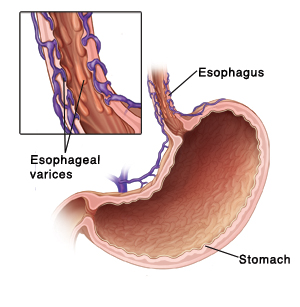
Esophageal Varices
Esophageal varices are enlarged veins at the lower end of the esophagus. The esophagus is the tube that carries food from your mouth to your stomach. Varices most often occur because of problems with blood flow in the liver caused by chronic liver disease. Normally, a blood vessel called the portal vein carries blood from the digestive organs to the liver. But with liver disease, blood flow can be blocked due to scarring of the liver. This increases the blood pressure in the portal vein (a condition known as portal hypertension). Blood then backs up in nearby veins in the esophagus and stomach, causing varices. Varices are a serious and deadly problem. Treatment is needed to prevent them from bursting (rupturing) and bleeding. If bleeding occurs, it can cause death.
Symptoms of esophageal varices
Symptoms don't occur unless the varices are bleeding. This is an emergency problem. If you have any of the following symptoms, get medical care right away:
-
Vomiting blood or vomit that looks like coffee grounds
-
Black, tarry, or bloody stools
-
Feeling lightheaded, or fainting (loss of consciousness)
Diagnosing esophageal varices
You’ll likely be checked for varices if you have liver disease or other health problems that can cause them. Your healthcare provider will ask about your symptoms, recent illnesses, and health history. You’ll also be examined. Tests are then done to confirm the problem. Tests can include:
-
Upper endoscopy. This is done to see inside the upper digestive tract. During the test, an endoscope is used. This is a thin, flexible tube with a tiny camera on the end. It’s inserted through your mouth. It’s then guided down through your esophagus, stomach, and first part of your small intestine. This allows the provider to check for varices and find any bleeding.
-
Imaging tests. These provide pictures of the liver or blood flow in the liver. They allow the provider to check for enlarged veins around the liver and assess the risk of bleeding. Common imaging tests done include ultrasound and CT scans.
Treating esophageal varices
The goal of treatment is to reduce the risk of bleeding or to control bleeding. Treatment can include 1 or more of these:
-
Medicines. These may be prescribed to lower the blood pressure inside the enlarged veins. This reduces the risk of bleeding. Beta-blockers are the most common medicine used.
-
Endoscopic therapy. These are treatments for enlarged or bleeding veins that are done using an endoscope. With ligation, small rubber bands are placed around the veins to close them off and stop any bleeding. With sclerotherapy, a blood-clotting medicine is injected into the veins to cause scarring and shrink them.
-
Balloon tamponade. A tube with a balloon is guided down into your esophagus and stomach. The balloon is then filled with air. This puts pressure on enlarged or bleeding veins to control bleeding. This is a short-term (temporary) way to control bleeding until other treatments are available.
-
Surgery. This may be done to place a tube-like device (stent) in the liver. The stent helps redirect blood flow in the liver to lower the blood pressure in enlarged veins. Sometimes, the enlarged veins may be connected to other nearby veins to redirect blood flow. In severe cases, a liver transplant may be needed. For this surgery, a diseased liver is replaced with a healthy liver from another person.
Follow-up
Regular visits with your healthcare provider are needed to check for bleeding of the varices. If bleeding occurs, it's likely to occur again. More treatments will then be needed in the future. Once endoscopic therapy (banding) is done, regular follow-up endoscopic scans with banding are done to completely get rid of the varices. If you're given medicines to take by mouth, take them as directed. Work closely with your provider to manage your condition. Know when to get emergency care.