Parotidectomy
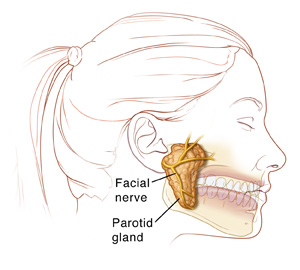
The parotid gland is a large salivary gland near the ear. It helps make and control the release of saliva. There's one on each side of your face.
The facial nerves pass through each parotid gland. Each nerve controls the muscles on that side of the face. If a tumor forms in the parotid gland, it can press on the facial nerve, causing discomfort and pain. Part or all of one side of the face may be weak or paralyzed.
To treat a parotid tumor, part or all of the gland is removed. This surgery is called parotidectomy. The amount of the gland removed depends on how much of it is affected. Your healthcare provider may not know how much needs to be taken out until surgery is done. If the cancer has spread deep into the parotid, the whole gland will need to be taken out. This is called a total parotidectomy. The facial nerve and nearby tissues may also need to be removed.
Types of tumors
Most parotid tumors are not cancer. They're benign. A benign tumor may grow larger, but it will not spread to other parts of the body. But some parotid tumors are cancer. These can become metastatic, meaning they can spread to other parts of the body. Whether the tumor is benign or cancer, part or all of the parotid gland will be removed. If a tumor is cancer, nearby tissues or lymph nodes may also be removed. Sometimes other cancer treatments, like radiation therapy, are needed.
Protecting the facial nerve
During this surgery, steps are taken to protect the facial nerve. This may include using a device called a facial nerve monitor to sense activity in and around the nerve. This helps to map the exact location of the nerve, so the healthcare provider can prevent touching it during surgery.
In some cases, the facial nerve can’t be completely protected. The facial nerve helps you move your lips, close your eye on that side, and wrinkle your nose. You and your healthcare provider will discuss whether your facial nerve is likely to be affected by the surgery, what changes you might have, and what your choices are. Some choices might include skin grafts, nerve grafts, and plastic or reconstructive surgery.
Getting ready for surgery
Get ready for the procedure as you have been instructed. Be sure to tell your healthcare provider about all medicines you take. This includes over-the-counter medicines, street drugs, and marijuana. It also includes herbs, vitamins, CBD, and other supplements. You may need to stop taking some or all of them before surgery. Also, follow any directions you’re given about not eating or drinking before surgery.
The day of surgery
The surgery may take 3 to 5 hours.
Before the surgery begins
-
An IV (intravenous) line is put into a vein in your arm or hand. This line is used to give you fluids and medicines.
-
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine puts you into a deep sleep so you don't feel pain.
During the surgery
-
The surgeon makes a cut (incision) from the front of your ear to partway down your neck to expose the parotid gland.
-
The facial nerve is located. Great care is taken to prevent harming this nerve. A facial nerve monitor (a machine with a small sensor that's put on your cheek) may be used to map the nerve’s exact location. It makes noise when the nerve is set off. This helps prevent damage.
-
The gland is removed.
-
If cancer is present, a margin (rim) of healthy tissue around the gland is also removed. Nearby lymph nodes may also be taken out.
-
The incision is closed with stitches (sutures), surgical glue, or both.
-
A small tube (drain) may be put into the surgical area. This drains blood and fluid that may build up after surgery. The drain will likely be removed before you go home.
After the surgery
You'll be taken to a recovery room to wake up from the anesthesia. You may feel sleepy and nauseated at first. You will be given medicine to control pain. You may then be taken to a hospital room to stay for a day or so. Your surgeon will determine if you stay in the hospital and for how long. It depends on the extent of the surgery and your condition.
Once you are ready to go home, you'll be released to an adult family member or friend. Have someone stay with you for a few days as your healing begins. If you’re sent home with a drain, you will be shown how to care for it.
Recovering at home
Once at home, follow the instructions you have been given. Keep in mind that nerves take time to heal. It could be weeks or months before the facial nerve returns to normal. Discuss what to expect with your healthcare provider. During your recovery:
-
Take all prescribed medicine as directed.
-
Sleep with your head raised above the level of your heart for 3 to 5 days after the surgery. This helps reduce swelling.
-
Limit activity as directed. Your healthcare provider will tell you when you can return to your normal activities and routine.
-
Don't drive until you are no longer taking pain medicines that make you drowsy.
-
Care for your bandage and incision as directed. Don't get your incision or bandage wet until your healthcare provider says it’s OK.
-
Check your incision daily for symptoms of infection listed below.
When to call your healthcare provider
Be sure you have a contact number for your healthcare provider. Ask how to get help after office hours and on weekends and holidays. After you get home, call if you have any of these:
-
Chest pain or trouble breathing (call 911)
-
Fever of 100.4° F ( 38° C) or higher, or as directed by your healthcare provider
-
Pain that gets worse or is not relieved by pain medicine
-
Symptoms of infection at the incision site, such as increased redness or swelling, warmth, pain that gets worse, or fluid draining
-
Severe facial swelling or weakness
- New trouble smiling, blinking, or drinking fluids
-
Trouble eating or drinking
-
Severe nausea or vomiting
-
Warmth, pain, redness, or swelling in an arm or leg
Follow-up care
During follow-up visits, your healthcare provider will check on your healing. If you have drains that need to be removed, this may be done 1 to 2 days after surgery. Stitches or staples will likely be removed 5 to 10 days after the surgery. If your surgery was done to treat cancer, you may need more treatment. Your healthcare provider can tell you more.
Risks and possible complications
Risks of parotidectomy include:
-
Infection
-
Bleeding, including a collection of blood under skin (hematoma)
- Pain
- Wound healing problems
-
Scars
-
Ear numbness
- Face numbness and drooping
-
Injury to the facial nerve or some of its branches, which may result in permanent weakness or paralysis. This often gets better over time as the nerves slowly heal.
- Nerve damage that can cause problems moving your tongue, talking, or swallowing
-
Buildup of fluid around the wound that causes swelling (seroma)
- Buildup of saliva under the skin near the wound or through the wound (sialocele)
-
Sweating and redness on the affected side of the face while eating. This is because of changes to the nerves. This condition is common. It's called Frey syndrome or gustatory sweating.
-
Inability to remove the entire tumor, meaning that you will need further cancer treatment
-
The cancer returns
-
Risks of anesthesia that the anesthesiologist will discuss with you
-
Changes in the way you look
- First bite syndrome. This is sharp pain or a cramping sensation in the parotid area during chewing when starting to eat.