Treating Bladder Cancer: Intravesical Therapy
Sometimes bladder cancer is treated by putting medicines that kill cancer cells right inside the bladder. This is called intravesical therapy. This treatment doesn't affect your whole body. It only damages the cancer cells in the lining of your bladder. It might be used for nonmuscle invasive bladder cancer:
- Shortly after a type of surgery called TURBT (transurethral resection of bladder tumor) to kill any cancer cells left in the bladder.
- To treat tumors that are small (stages 0 and I), slow-growing (low grade), and only in the lining of the bladder.
- As a long-term treatment for cancer that's big and fast-growing. Or if there's more than one tumor.
- After radiation and chemo for stage II tumors if surgery can't be done.
Medicine in your bladder
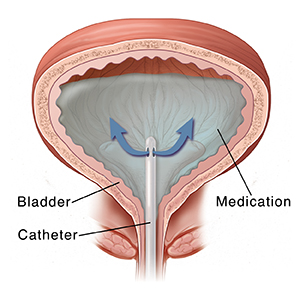
This treatment is often done in a healthcare provider’s office. Or it may be done at an outpatient clinic. A soft, thin, flexible tube (catheter) is put into the urethra. It is then passed to the bladder. The catheter fills the bladder with the liquid medicine.
Most often, an immunotherapy medicine called BCG (Bacillus Calmette-Guerin) is used. BCG is a type of very weak bacteria. It boosts your immune system so that it kills the cancer cells. It has to come in contact with the cancer cells to work. This makes it a good choice for intravesical therapy. But since the early 2010s, there has been a limited supply of BCG in the U.S. and worldwide. BCG supply isn't expected to increase for a few more years. Talk with your provider about your treatment choices.
A chemo medicine might be used if BCG doesn't work or isn't a treatment choice. Mitomycin and gemcitabine are the medicines most often used. There are also other chemo medicines that might be used. The chemo might be heated before it's put in your bladder. This is called hyperthermic intravesical chemo. The heat might help the medicine get into the cancer cells.
During treatment
After the medicine is put in, you'll need to keep it in your bladder for 1 to 2 hours. The catheter might be left in. It's used to take out the medicine after treatment. Then it's removed. Sometimes the catheter is taken out after the medicine is put in. Then you'll pee after the 1 to 2 hours are over. You may need to pour bleach in the toilet after you pee if BCG is used. This kills any bacteria that may be left over.
Your treatment plan
There are many schedules used for intravesical therapy. Your healthcare provider will talk with you about the plan that's best for you.
-
BCG. The first cycle is often weekly for 6 to 8 weeks. During this time, you may be given antibiotics to help prevent infection. Then you may need follow-up treatments for up to 3 years. This is called maintenance BCG therapy. This helps keep the cancer from coming back.
-
Chemo. These medicines are given weekly for 6 weeks. You might have 2 cycles. Treatment seldom lasts more than 1 year.
When all the treatments are done, you may have tests every few months. This is to see how well the treatment has worked.
Side effects of treatment
-
Intravesical BCG. This tends to cause flu-like symptoms for a few days after treatment. This includes fever, chills, aches, and severe tiredness (fatigue). You might see blood in your pee or need to pee more often and right away (urgency). Or you may have a burning feeling in your bladder. This is common.
-
Intravesical chemo. This can cause a burning feeling in your bladder and blood in your pee.
Risks and possible complications
Possible side effects include:
-
Bladder infection
-
Blood in the pee
-
Bladder irritation (burning feeling, need to pee often, pain when peeing)
-
Flu-like symptoms, such as fever and chills
-
Scarring of the bladder (rare)
-
Blood infection with BCG (very rare, but can happen even years after treatment.)
When to call your healthcare provider
Call your provider right away if you:
- Have a fever of 100.4°F (38°C) or higher, or as advised by your provider
Ask your provider what other problems you should watch for. And ask what you should do if you have them. Know how to contact the provider's office any time. This includes after office hours and on weekends and holidays.