Treatment for Your Child’s Biliary Atresia: Kasai Procedure
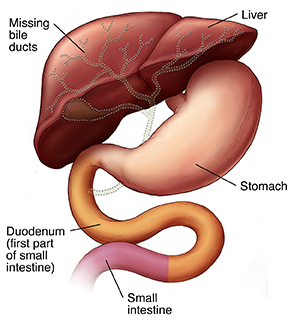
Biliary atresia is a serious liver problem that occurs in young babies. It involves a problem with the bile ducts. These are the tubes that drain bile from the liver into the small intestine. In children with biliary atresia, the bile ducts are damaged, scarred, missing, blocked, or not shaped correctly. Bile is not able to flow into the intestine, so it builds up in the liver, causing damage. Treatment must be done as soon as possible. Biliary atresia is treated with surgery. Even if this surgery goes well, your child will likely need a liver transplant in the future.
Understanding the Kasai procedure
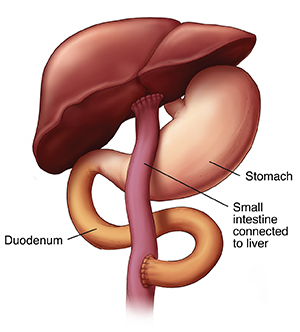
Surgery for biliary atresia is called the Kasai procedure. During this surgery, the surgeon removes any problem bile ducts outside the liver. The small intestine is then attached to the liver. This provides a path that can allow bile to drain from the liver. The details of the surgery for your child will depend on the condition of your child’s liver. The surgeon can tell you more. Surgery is not a cure for biliary atresia. It won’t work if the bile ducts inside your child’s liver are damaged or missing. But in many cases, it does help the liver work better for many years.
Building your child’s strength before surgery
Your child’s surgery will likely take place shortly after the diagnosis of biliary atresia. To help make sure your child is strong enough for surgery:
-
You may be asked to feed your child special formula and vitamins.
-
If you’re breastfeeding, continue. Stop feedings only when your healthcare provider tells you to.
-
Before surgery, a nasogastric (NG) tube may be placed to give your child food. This is a small, soft tube that is inserted into your child’s nose. It leads down the esophagus and into the stomach. Food is then sent through the tube into the stomach. If the NG tube is needed, the healthcare provider will tell you more.
The day of surgery
-
Before surgery. Don't give your child anything to eat or drink for 4 to 6 hours before surgery. Follow all other instructions you are given.
-
During surgery. You will stay in a waiting room nearby during your child’s surgery. Your child will be given medicine to make them sleep during the surgery. How long the surgery will take depends on your child’s condition.
What to expect after surgery
-
Your child will stay in the hospital for 5 days or longer. During this time, the nursing staff will care for your child.
-
Your child will have frequent blood tests. These check the function of the liver.
-
Tubes will help drain fluid from around your child’s incision. This helps the incision heal.
-
Your child won’t be able to eat for 2 to 3 days after surgery, when the intestines start working again. During this time, your child will be given nutrition through an IV (intravenous) line. Once your child can eat again, they may be able to take food by mouth, or fed by NG tube for a time.
-
Your child may be given corticosteroid medicine. This helps decrease irritation and swelling of the bile ducts in your child’s liver. This medicine may be given short-term or long-term.
Caring for your child after surgery
Even after surgery, your child’s liver won’t be fully back to normal. Your child will need special foods and medicine to help the liver do its work. The care steps listed below are needed after surgery, and likely for a long time after. Your child will need:
-
Feeding with breastmilk or special formula. These provide types of fats that are easier for the liver to absorb.
-
Supplements for vitamins A, D, E, and K. These are fat-soluble vitamins. Your child’s body can’t absorb these well without bile. The supplements may be needed for a long time. Or you may be able to stop giving them after a period of time.
-
Antibiotic medicine. Your child may need this for a few months after surgery. It helps prevent infection (cholangitis) caused by bacteria that travel from the intestines into the liver and bile ducts. Your child may be at risk for cholangitis after a cold or other illness. Cholangitis will be treated with antibiotics.
-
Bile acid replacement medicine. This helps improve bile flow. Your child may take this medicine for several years.
Long-term follow-up
Your child’s health needs to be closely watched. At first, you will need to visit your child’s healthcare provider often. As your child gets older, you may be able to visit less often. These visits may include:
-
Blood tests. These are done to measure liver function and nutrition levels.
-
An ultrasound exam. This uses harmless sound waves to create an image of the liver.
-
Other tests. Your child may need additional kinds of tests over time. Your child’s healthcare provider will tell you more about these.
-
Vaccines. Your child will need to have vaccines against common childhood diseases. Make sure your child gets a flu shot every year. Your child will also need vaccines for hepatitis A and B. These are liver diseases and can be much worse for a child who has biliary atresia.
In the future: a possible liver transplant
Many children with biliary atresia need a liver transplant at some point. This may be needed a few years after the Kasai procedure. Or, a transplant may not be needed for 10 years or more. Follow-up visits and tests help the healthcare provider determine whether a transplant is needed. The liver is an organ that can be donated by a living donor. This means another person may be able to donate a portion of their own liver. The removed portion grows back. If you want to know more about a living donor transplant, talk to your child’s healthcare provider.
When to call the healthcare provider
After your child’s surgery, call the healthcare provider right away if you notice any of the below:
-
Jaundice that gets worse, or comes back after treatment
-
Itching
-
Abdominal swelling or pain
-
Poor growth
-
Any signs of a vitamin deficiency, such as poor balance, inability to walk, bowlegs, or scaly skin
-
Bloody stool or vomit
-
Pale gray or white-colored stools
-
No bowel movement or watery bowel movements for more than 3 days
-
Confusion, extreme sleepiness, or loss of consciousness
-
Fever of 100.4ºF ( 38ºC) or higher, or as directed by your healthcare provider
-
Chills
-
Unusual bruising or bleeding
-
Redness, swelling, or fluid leaking from wounds