Understanding Cardiac Resynchronization Therapy (CRT)
Cardiac resynchronization therapy (CRT) is a treatment that may help you when your heart isn’t pumping as well as it should. This problem can be caused by heart failure, a condition in which the heart muscle has become weak. It can also be caused by an electrical problem that keeps the bottom pumping chambers of the heart (ventricles) from beating in sync. This is known as a bundle branch block. This can make heart failure worse.
When you have heart failure, fluid can build up in your lungs and your legs (edema). You may have less energy and be short of breath. These symptoms interfere with daily life.
CRT uses a small device to help improve the timing of the heart’s contractions. CRT can ease symptoms, improve your quality of life, and help you live longer.
How CRT Works
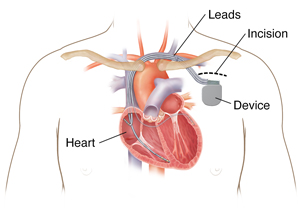
With CRT, a small electrical device (pacemaker or defibrillator) is put under the skin in the upper chest. This is a minor surgical procedure done at a hospital. It's not heart surgery. Wires from the device lead to the ventricles. The device sends electrical pulses to each ventricle at the same time. This keeps the ventricles beating in sync. This procedure is also called biventricular pacing or resynchronization pacing.
CRT can be done with 1 of 2 devices. The type of device used depends on the person’s needs. The devices are:
-
A biventricular pacemaker. This device helps the heart beat at a normal rate. It's called a biventricular pacemaker because a pacing wire is placed in both the right and left ventricle.
-
A biventricular ICD (implantable cardioverter defibrillator). This device is a biventricular pacemaker. But it can also treat fast, life-threatening heart rhythms. It does this by overdrive pacing or internally shocking dangerous heart rhythms. This resets them to a normal heart rhythm.
Reasons for CRT
Your healthcare provider may advise CRT if:
-
You have heart failure symptoms, and your heart doesn’t pump well.
- You have heart conduction problems, such as a bundle branch block.
-
The ventricles are not working together, and CRT may prevent heart failure symptoms.
-
Tests, such as an echocardiogram, show that your heart is weak and enlarged.
-
Medicine and lifestyle changes are not working well enough to control your heart failure.
Benefits of CRT
CRT won’t replace your other treatments. It’s part of a complete heart failure treatment plan. CRT helps a weakened heart do a better job of pumping blood out of the heart with each beat. This is so more blood and oxygen go to the rest of your body. This can prevent or decrease heart failure symptoms and improve survival. The device is put into your body during a low-risk procedure.
Not everyone with heart failure benefits from CRT. CRT improves symptoms in about 2 out of 3 people who get it. For those who have mild symptoms, it can also prevent heart failure from getting worse. With CRT, you may be more able to:
-
Return to daily activities, such as walking, carrying grocery bags, and climbing stairs
-
Have more energy to be active and do the things you enjoy
-
Breathe more easily when you lie flat, so you sleep better at night
-
Have less swelling in your ankles, feet, and abdomen (belly)
-
Make fewer visits to the hospital because of heart failure symptoms
-
Have fewer side effects from your heart failure medicines
- Live longer
Risks and possible complications
Like all medical procedures, having a CRT device implanted has some risks. These include:
-
Anesthesia reactions
-
Swelling or bruising in the upper chest area where the CRT device is placed
-
Bleeding
-
Infection
-
Heart rhythm problems
-
Collapsed lung
-
Nerve or blood vessel damage
-
Movement of the device or the device wires, which may need a second procedure
-
Mechanical problems with the CRT device
-
Kidney damage
-
Heart failure suddenly getting worse
- Twitching on one side of your chest (diaphragm stimulation)
-
Other risks related to your specific health condition
Life with CRT
If you have a CRT device, you may need to stay away from certain electronic devices and devices that have strong magnetic fields. These devices can interfere with how the CRT device works. You will need to stay away from CB radios, and very strong magnets, such as those used in MRI. However, depending on the type of device you have implanted, you may be able to undergo an MRI with certain precautions in place. Talk to your cardiologist and the radiologist to make sure it is safe. Retail store antitheft systems and security metal detectors are generally safe if you walk through without lingering or leaning against the detector.
Be careful when using cell phones and other electronic devices. Keep them at least 6 inches away from your CRT device. It's safest to hold all cell phones to the ear farther from your CRT device or use the speaker mode setting. Don’t carry your phone or electronic device in your chest pocket, over the CRT device. Experts advise carrying your cell phone and other electronics in a pocket or bag below your waist. Most cell phones and electronic devices don't interfere with CRT devices. But some cell phones and electronic devices, such as smart watches, use powerful magnets for wireless charging. These may interfere with the normal function of your CRT device. The magnet used for charging or other magnet accessories can also interfere with the normal function of your CRT device. These should be kept away from your CRT device when wirelessly charging or stored. Follow any other instructions given to you by your healthcare provider or from the manufacturer of your CRT device.
Your provider may give you a list of other devices and procedures to stay away from. Most people with CRT devices can still enjoy physical activity, including sports and exercise. Don't do any activities that could damage the CRT device and could cause it to stop working correctly. This could include impact sports, such as football. Ask your provider if an activity is safe to do if you have questions about it.
Don't drive until your healthcare provider says it's OK. The driving restriction is to be sure that your health condition does not cause a safety issue for yourself or others on the road. Ask your provider when it may be safe for you to continue to drive.
You will have regular appointments to see how the device is working and to check the battery life of your device. Some of the device tracking can be done using a home device that sends the information about your device to your healthcare provider's office over a telephone or internet connection. The battery or generator will have to be changed at some point. This is usually after 8 to 10 years. You will need another surgical procedure for this. Your provider will let you know as that time approaches.