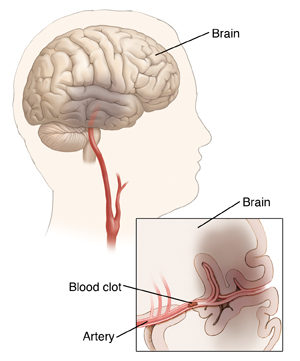
Thrombolytic Therapy for Stroke
An ischemic stroke occurs when blood flow to the brain is blocked. This is most often because of a blood clot in an artery in the brain or an artery leading to the brain. Treatment is needed right away to help dissolve the clot and restore normal blood flow. Restoring normal blood flow can limit damage to brain tissue and improve outcome. With thrombolytic therapy, a clot-busting medicine is used to dissolve the clot. The medicine may be given through an IV (intravenous) line. Or it may be directly sent to the site of the clot through a thin, flexible tube (catheter).
Before the treatment
-
People with certain health problems have increased risks for problems with thrombolytic therapy. For this reason, a detailed health history must be taken to check whether it's safe to have the treatment. Tell your healthcare provider about any health problems you have. The provider will also ask whether you’ve had specific problems, such as a past stroke, head injury, or bleeding in the brain.
-
Tell the healthcare provider about all medicines you take. Mention if you take blood thinners (anticoagulants). Also mention if you take over-the-counter medicines, vitamins, minerals, herbal medicines, or other supplements.
- Tell your provider about any allergies you may have, including allergy to contrast dye.
-
Tell your healthcare provider if you use alcohol or tobacco products so that they can give you the safest possible care.
-
Tell your healthcare provider if you are pregnant or if you are breastfeeding.
-
Tell your healthcare provider if you have had recent surgery or a head injury.
-
Certain tests need to be done before the treatment. These include blood tests and imaging tests, such as a CT or MRI scan of the brain.
-
Treatment with a thrombolytic must start within 4.5 hours after symptoms start.
-
To be eligible, you must have symptoms that continue plus a diagnosis of ischemic stroke.
-
Your blood sugar will be checked to rule out low blood sugar as cause of symptoms.
-
Two IV lines will be placed in your hand or arm.
-
Your blood pressure may be lowered before giving a thrombolytic.
During the treatment
Through an IV line
Clot-busting medicine is sent through an IV line in your arm or hand. It will travel through your blood until it reaches the clot. You’ll be watched closely throughout the treatment. You will stay in an intensive care unit or a stroke unit for at least 24 hours for monitoring. Your blood pressure must remain below 180/105 mmHg for the first 24 hours after therapy.
Through a catheter
-
You are given medicine to numb the site where the catheter will be inserted. This is often the groin area.
-
The radiologist makes a small hole (puncture) in the artery. Then the provider puts the catheter into the hole. Using X-rays, the provider carefully guides the catheter through the artery.
-
Contrast dye is injected through the catheter into the artery. This helps the artery show up clearly on X-ray images. The radiologist uses these images as a guide. They move the catheter through the artery to the clot.
- When the catheter reaches the clot, the radiologist adds medicine or uses a device to dissolve the clot.
- When the procedure is complete, the radiologist removes the catheter.
- The staff will put pressure on the insertion site for a time to stop any bleeding. Once the bleeding has stopped, they will put a very tight bandage on the site.
After the treatment
After the treatment, you’ll need to stay in the hospital for at least several days. More imaging tests will be done to check how well the clot is dissolving. Other tests may also be done to help find the cause of the stroke.
If you have the catheter-directed thrombolysis, you will be taken to a recovery area to lie flat for a few hours. Your healthcare provider will talk with you about the results soon after the procedure. Depending on your test results and your health condition, you will either be discharged home or stay in the hospital.
Once you are home:
-
Don’t drive for 24 hours or as advised by your provider.
-
Don't walk, bend, lift, or take stairs for 24 hours or as advised by your provider.
-
Don't lift anything over 5 pounds (2.27 kg) for 7 days.
Follow any other instructions from your healthcare provider.
Risks and possible complications
-
Bleeding in the brain or elsewhere in the body
-
Allergic reaction to the clot-busting medicine. This includes skin rash, itching, or swelling of your face or tongue.
- Sharp pain or pain at the catheter insertion site that gets worse
-
Chest pain or pressure
-
Severe headache
-
Shortness of breath
-
Heart problems that get worse
-
Dizziness or lightheadedness
-
Nausea and vomiting
-
Death
Follow-up care
Recovery from a stroke can take several months or longer. Keep all follow-up appointments with your healthcare provider. These are needed to keep track of your health and how well you are recovering. You may need other treatments, such as medicines, rehab (rehabilitation), and surgery in the future. Your healthcare provider will talk about these with you as needed.
Call 911
Call 911 or go to an ER (emergency room) right away if you have any of these signs of a stroke:
-
Sudden, unexplained numbness or weakness on a side of the body
-
Problems seeing, double vision, or blurry vision
-
Sudden confusion or problems with speech
-
Sudden dizziness, trouble walking, or problems with balance
-
Sudden, severe headache
B.E. F.A.S.T. for stroke
B.E. F.A.S.T. is an easy way to remember the signs of a stroke. When you see these signs, you will know that you need to call 911 fast.
B.E. F.A.S.T. stands for:
- B is for balance. Sudden loss of balance or coordination.
-
E is for eyes. Vision changes in 1 or both eyes.
-
F is for face drooping. One side of the face droops or is numb. When the person smiles, the smile is uneven.
-
A is for arm weakness. One arm is weak or numb. When the person lifts both arms at the same time, 1 arm may drift downward.
-
S is for speech difficulty. You may notice slurred speech or trouble speaking. The person can't repeat a simple sentence correctly when asked.
-
T is for time to call 911. If someone shows any of these symptoms, even if they go away, call 911 right away. Make note of the time the symptoms first appeared.
If you are at risk for having a stroke:
-
Keep a list of important phone numbers next to your phone or in your cell phone list of contacts. Include your healthcare provider and relatives or friends you want to be contacted.
-
Carry a list of all medicines you take and the dosages of each, in your wallet. Include over-the-counter medicines, vitamins, and supplements.
-
Write a brief health history, including any other medical problems you have had and the dates. Keep this with the medicine list.