Nonalcoholic Fatty Liver Disease (NAFLD)
Nonalcoholic fatty liver disease (NAFLD) is a common disease of the liver. It occurs when you have too much fat in the liver. If NAFLD is severe, it can cause liver damage that seems like the damage caused by drinking too much alcohol. But NAFLD is not caused by drinking alcohol. This sheet tells you more about NAFLD and how it can be managed.
How the liver works
The liver is an organ in the upper right side of the belly (abdomen). It has many important jobs. These include:
-
Breaking down (metabolizing) proteins, carbohydrates, and fats
-
Making a substance called bile that helps break down fats
-
Storing and releasing sugar (glucose) into the blood to give the body energy
-
Removing toxins from the blood
-
Helping with blood clotting
Understanding NAFLD
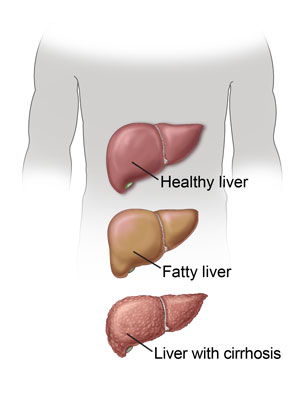
A healthy liver may contain some fat. But if too much fat builds up in the liver, this causes NAFLD. NAFLD can be mild, causing fatty liver. Or it can be more severe and have inflammation as well as excess fat. This can cause nonalcoholic steatohepatitis (NASH).
-
Fatty liver. With fatty liver, the liver simply has more fat than normal. This extra fat usually doesn't harm the liver.
-
NASH. With NASH, the fatty liver becomes inflamed over time. NASH is serious because it can lead to scarring of the liver (fibrosis). Over time, the scarring may lead to cirrhosis of the liver. This can eventually cause liver failure or liver cancer.
Causes and risk factors for NAFLD
Doctors don't know what causes NAFLD. But certain things make the problem more likely to happen. These include:
-
Obesity
-
Prediabetes or diabetes
-
Polycystic ovary syndrome (PCOS)
-
High blood pressure (hypertension) and heart disease
-
High levels of fat found in the blood (cholesterol and triglycerides)
-
Taking certain medicines
Symptoms of NAFLD
Most people with NAFLD have no symptoms. If symptoms do occur, they can include:
-
Tiredness
-
Weakness
-
Weight loss
-
Loss of appetite
-
Upset stomach (nausea) and vomiting
-
Belly pain and cramping
-
Yellowing of the skin and eyes (jaundice)
-
Dark urine
-
Light-colored poop (stool) that looks gray
-
Swelling in the belly or legs
Diagnosing NAFLD
Your healthcare provider may think you have NAFLD if routine blood tests show high levels of liver enzymes. This may mean you have a liver problem. You may need 1 or more imaging tests, such as an ultrasound, CT, or MRI. You may need more blood tests to look for other causes of liver disease. You may also need a liver biopsy. During this test, a hollow needle is used to remove a tiny tissue sample from your liver. This tissue is then checked in a lab. This test can find signs of damage to liver tissue. It can also help figure out the cause of the damage and tell the difference between fatty liver and NASH.
Treating NAFLD
Treatment for NAFLD varies for each person. The best early treatment is to treat any conditions that are causing metabolic syndrome. This syndrome is a group of conditions that includes:
-
High blood pressure
-
High levels of cholesterol and triglycerides
-
Being overweight or obese
-
Diabetes
Your healthcare provider will monitor your health and treat any symptoms or underlying health problems you have. Your provider will also work with you to control your risk factors. This will make liver damage less likely. In fact, treating those underlying conditions can often improve liver disease. You may need to take certain medicines, but no medicine will cure NAFLD. This is why treating the underlying conditions is most important. Your plan may include:
-
Losing excess weight
-
Getting regular exercise
-
Controlling diabetes
-
Controlling high cholesterol or triglyceride levels
-
Taking medicines and vitamins as prescribed by your provider
-
Not smoking
-
Not drinking alcohol
-
Eating a healthy diet
Living with NAFLD
If NAFLD is caught early, it can be managed with treatment. Your healthcare provider will discuss further treatment choices with you as needed. Follow up with all treatment suggestions. Ask your providers for help if you have trouble managing any of their advice.
Be sure to ask your provider about advised vaccines. These include vaccines for viruses that can cause liver disease.