Endometrial Cancer
Introduction
Endometrial Cancer: Introduction
What is cancer?
Cancer is when cells in the body change and grow out of control. To help you understand what happens when you have cancer, let’s look at how your body works normally. Your body is made up of tiny building blocks called cells. Normal cells grow when your body needs them, and they die when your body does not need them any longer.
Cancer is made up of abnormal cells that grow even though your body doesn’t need them. In most cancers, the abnormal cells grow to form a lump or mass called a tumor. If cancer cells are in the body long enough, they can grow into (invade) nearby areas. They can also break off and spread to other parts of the body (metastasis).
What is endometrial cancer?
Endometrial cancer starts in the cells that form the inner lining of the uterus (which is called the endometrium).
You may hear endometrial cancer called uterine cancer. It's actually one of two main types of uterine cancer. The other is called uterine sarcoma. It starts in the muscle layer of the uterus, not the lining.
Endometrial cancer is the most common type of cancer in the uterus. It usually takes years to develop. It most often occurs in women who have already gone through menopause. It is highly curable when found early.
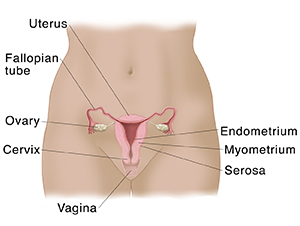
Understanding the uterus
The uterus is an organ. It’s part of the female reproductive system. You may know it as the womb. The uterus is usually pear-shaped and about the size of a fist. It is located in the lower belly (pelvic area) between your bladder and your rectum. Your uterus is connected to your fallopian tubes. These tubes help carry eggs from your ovaries into the uterus. The small opening that connects the uterus to your vagina is the cervix.
The uterus is made up of three layers:
-
Endometrium. This is the inner lining.
-
Myometrium. This is the middle muscle layer.
-
Serosa. This is the outer smooth layer.
The uterus protects a growing baby during pregnancy. During labor, the myometrium muscle tissue helps push the baby out through the cervix. The smooth serosa makes it easy for the uterus to move in the pelvis as needed.
Understanding the endometrium
In women who still have their periods, one of the ovaries releases an egg into a fallopian tube each month. During this time, the endometrium becomes thicker as it gets ready to receive a fertilized egg. If the egg connects with a male sperm cell, this fertilized egg attaches to the endometrium. If the egg is not fertilized, it travels out of the uterus along with the endometrial lining as a woman's period (menstrual flow).
How endometrial cancer spreads
If endometrial cancer spreads, it tends to grow into the muscle layer of the uterus, the myometrium, and then may go to places near the uterus. This may be the fallopian tubes, ovaries, cervix, vagina, or lymph nodes. It can also spread to the bladder or rectum. Advanced stages of endometrial cancer can spread as far as the bones and lungs. Most cases of endometrial cancer are found in the early stages before they have spread outside the uterus.
Cancer that spreads to other parts of the body is called metastatic cancer. The process is called metastasis. Metastasis is a complex process. The cancer cells of the tumor grow into other tissues, blood vessels, and the lymph system. They then travel through the bloodstream or lymph system to reach other parts of the body where they grow into new tumors.
Talk with your healthcare provider
If you have questions about endometrial cancer, talk with your healthcare provider. Your healthcare provider can help you understand more about this cancer.
Symptoms
Endometrial Cancer: Symptoms
What are the symptoms of endometrial cancer?
The main symptom of endometrial cancer is unusual vaginal bleeding. This occurs in almost all people with endometrial cancer. The bleeding may include:
-
Changes in the kind of bleeding during periods, such as a very long period or heavy bleeding
-
Bleeding between periods
-
Any vaginal bleeding after menopause
For most people, abnormal vaginal bleeding is the only symptom they have. But other symptoms may include:
-
Non-bloody vaginal discharge
-
Pain when urinating
-
Pain during sex
-
Pain, pressure, or a lump in the pelvic area or lower belly (lower abdomen)
-
Losing weight without trying
When to see your healthcare provider
Tell your healthcare provider if you have any unusual bleeding from the vagina. Tell them if you have any bleeding at all after menopause. Even if it is just a bit of spotting or slight bloody discharge, it is very important to let your healthcare provider know, as this small amount of bleeding may be the only sign of a problem.
Some people develop endometrial cancer while they are entering menopause. During this time, periods may get heavier or lighter. This may not be a symptom of menopause. Make sure to tell your healthcare provider about any change in vaginal bleeding during this time.
Some of these symptoms may be caused by other health problems. But it is important to see your healthcare provider if you have these symptoms. Only a healthcare provider can tell if you have cancer.
Treatment Choices
Endometrial Cancer: Treatment Choices
There are various treatment choices for endometrial cancer. Which may work best for you? It depends on a number of factors. These include the location and stage of the cancer. Factors also include your age, overall health, and what side effects you’ll find acceptable. The good news is that endometrial cancer can often be cured.
Learning about your treatment options
You may have questions and concerns about your treatment options. You may also want to know how you’ll feel and function during and after treatment, and if you’ll have to change your normal activities.
Your healthcare provider is the best person to answer your questions. He or she can tell you what your treatment choices are, how successful they’re expected to be, and what the risks and side effects are. Your healthcare provider may advise a specific treatment. Or he or she may offer more than one, and ask you to decide which one you’d like to use. It can be hard to make this decision. It's important to take the time you need to make the best decision. Get any questions answered and learn as much as you can so you can make the decision that feels right for you.
Understanding the goals of treatment for endometrial cancer
Treatment can often cure endometrial cancer. It usually involves surgery to remove the uterus and the cancer in it.
Types of treatment for endometrial cancer
Treatment options include:
-
Surgery. Surgery is used to remove the uterus and the cervix. This is called a hysterectomy. It's the most common treatment for endometrial cancer. In most cases, the ovaries and fallopian tubes are removed, too. If the cancer has spread from the uterus to nearby tissues, part of the vagina and/or lymph nodes may also be removed.
-
Radiation therapy. This treatment kills cancer cells with high-energy X-rays. Radiation may be used after surgery to kill any cancer cells that may have been missed.
-
Chemotherapy. This treatment uses one or more medicines to kill cancer cells or shrink tumors. They work by attacking rapidly growing cells. Chemo may be given after surgery if the cancer is a type that tends to come back. It may also be used along with radiation in woman who cannot have surgery.
-
Hormone therapy. Medicines can be used to keep hormones from being made or stop their ability to help cancer cells grow. Hormone therapy may be used in women who cannot have surgery or radiation, or in women who have endometrial cancer that has spread to other parts of the body. It can also be used to treat the cancer without taking out the uterus in women who want to preserve fertility.
-
Biologic therapy. This is also known as immunotherapy. It uses medicines that work like chemicals that your body’s immune system makes. They help your immune system fight the cancer. It may be used along with chemo in women who have more advanced stages of endometrial cancer.
Your healthcare provider may suggest that you have more than one of these types of treatment. This is sometimes called combination therapy.
Clinical trials
Newer types of treatment may be available only through a research study. These studies are called clinical trials. Talk with your healthcare provider about what clinical trials may be an option for you. The National Cancer Institute can help you and your healthcare provider find appropriate trials.
Making a decision
Deciding on the best plan may take some time. At first, thinking about treatments options may seem overwhelming. Talk with your doctors and nurses. Make a list of questions. Consider the benefits and possible side effects of each option. Talk with your healthcare provider about how much time you can take to explore your options. You may want to get another opinion before deciding on your treatment plan. In fact, some insurance companies may require a second opinion. In addition, you may want to involve your family and friends in this process.