Chronic or Acute Pain
Saint Luke’s pain management experts provide diagnosis and treatment for patients suffering from chronic or acute pain. Our team focuses on creating individualized treatment plans, decreasing patients' pain and increasing their mobility, as well as reducing or eliminating patients' dependency on pain medication.
Our multidisciplinary team involves doctors and clinicians from a number of specialties, including anesthesiology, physical medicine, rehabilitation, and physical and occupational therapy.
Saint Luke’s provides:
- Precision spinal diagnostics
- Interventional pain management
- Psychological management
- Physical therapy
When traditional interventions are unable to relieve patients’ pain, Saint Luke’s pain management experts offer a new minimally invasive ablation therapy.
This treatment, called Cooled Radiofrequency Ablation (also Cooled RF or CRF), directly targets the sensory nerves causing pain. The procedure takes less than an hour, and patients resume normal activities within a few days.
Understanding Chronic Pain
Understanding Chronic Pain
Chronic means ongoing. Pain is called chronic when it lasts over a long period of time—at least 3 months. This includes pain that you feel regularly, even if it comes and goes. Chronic pain may be due to continuing injury or disease. Or it may be due to problems with the body’s pain-control system. An example of this is fibromyalgia.
Chronic stimulus
Chronic pain may be from ongoing arousal of the body's pain system. The cause may be an untreated injury or health problem. Common examples of these are:
- Joint degeneration (arthritis)
- Back injury
- Nervous system damage (neuropathic pain)
- Headaches
With this type of pain, both the pain and the condition that is causing it must be treated.
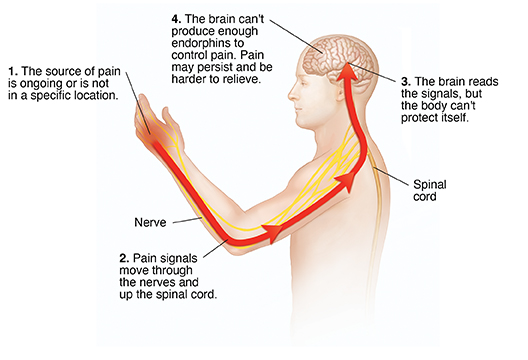
Chronic pain syndrome
In some cases, no cause can be found for a person's chronic pain. Some people with chronic pain develop chronic pain syndrome. In addition to the pain, this can include:
- Anxiety
- Depression
- Anger
- Changed lifestyle
It's important to talk with your healthcare team about these. You will need treatment for these problems in addition to treatment for pain.
Spinal Cord Compression
What is spinal cord compression?
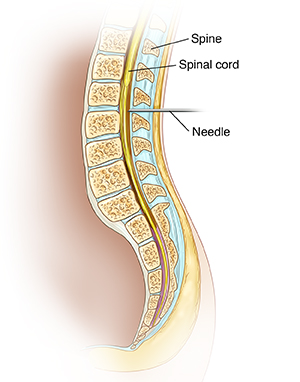
Spinal cord compression is caused by any condition that puts pressure on your spinal cord. Your spinal cord is the bundle of nerves that carries messages back and forth from your brain to your muscles and other soft tissues. As your spinal cord travels down your back, it's protected by a stack of backbones called vertebrae. They also hold your body upright. The nerves of your spinal cord run through the openings between the vertebrae and out to your muscles.
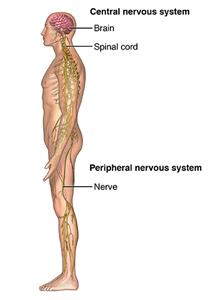
Spinal cord compression can occur anywhere from your neck (cervical spine) down to your lower back (very top of lumbar spine). Symptoms include numbness, pain, weakness, and loss of bowel and bladder control. Depending on the cause of the compression, symptoms may develop suddenly or gradually. They may require anything from supportive care to emergency surgery. If compression becomes severe, a condition called myelopathy may happen. Myelopathy leads to symptoms, such as problems with walking, pain, and numbness.
What causes spinal cord compression?
One of the most common causes of spinal cord compression is the gradual wear and tear on the bones of the spine. This is known as osteoarthritis. People who develop spinal cord compression from this are usually older than 50.
Other conditions that may cause spinal cord compression can develop more quickly, even very suddenly. These can occur at any age:
- Abnormal spine alignment (scoliosis)
- Injury to the spine
- Spinal tumor
- Certain bone diseases
- Rheumatoid arthritis
- Infection
What are the symptoms of spinal cord compression?
Symptoms of spinal cord compression can develop quickly or slowly. It depends on the cause. Injuries may cause immediate symptoms. Tumors or infections may cause symptoms that develop over days or weeks. Wear and tear of the spine may take years to cause symptoms.
These are common symptoms:
- Pain and stiffness in the neck, back, or lower back
- Burning pain that spreads to the arms, buttocks, or down into the legs (sciatica)
- Numbness, cramping, or weakness in the arms, hands, or legs
- Loss of sensation in the feet
- Trouble with hand or leg coordination
- "Foot drop," weakness in a foot that causes a limp
- Loss of sexual ability
Pressure on nerves in the lumbar region (lower back) can also cause more serious symptoms known as cauda equina syndrome. If you have any of these symptoms, you need to get medical care right away, typically in the emergency room:
- Loss of bowel or bladder control
- Severe or increasing numbness between the legs, inner thighs, and back of the legs
- Severe pain and weakness that spreads into one or both legs, making it hard to walk or get out of a chair
How is spinal cord compression diagnosed?
To diagnose spinal cord compression, your healthcare provider will ask you questions about your symptoms and do a complete physical exam. During the exam, they will look for signs of spinal compression, such as loss of sensation, weakness, and abnormal reflexes. Tests that help with your diagnosis may include:
- X-rays of your spine. These may show bone growths called spurs that push against spinal nerves. X-rays may also show an abnormal alignment of your spine.
- Special imaging tests of your spine. A CT scan or MRI will give a more detailed look at the spinal cord and the structures surrounding it.
- Other studies. These may include a bone scan, a special X-ray or CT scan taken after injecting dye into the spinal column (myelogram), and electromyography (EMG), an electrical test of muscle activity.
How is spinal cord compression treated?
The medical team involved in treating your spinal cord compression may include arthritis specialists, bone surgeons, nerve specialists, and physical therapists. Treatment depends on the cause and your symptoms. It may involve medicines, physical therapy, injections, and surgery. Except in cases of emergency, such as cauda equina syndrome or a broken back, surgery is usually the last resort.
- Medicines may include nonsteroidal anti-inflammatory drugs (NSAIDs) that relieve pain and swelling and steroid injections that reduce swelling.
- In more acute spinal cord compression, high-dose steroids are used to save nerve cells until other treatment can be given.
- Radiation therapy may be used to shrink tumors that are compressing the spinal cord.
- Physical therapy may include exercises to strengthen your back, abdominal, and leg muscles. You may learn how to do activities more safely. Braces to support your back or a cervical collar may also be helpful.
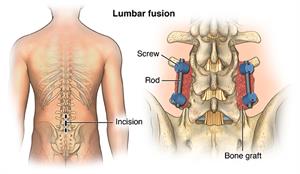
- Surgical treatments include removing bone spurs and making the space between vertebrae wider. Other procedures may be done to ease pressure on the spine or fix fractured vertebrae. The back may also be stabilized by fusing some of the vertebrae together.
- Some other treatments that may be helpful for some people are acupuncture and chiropractic care.
What can I do to prevent spinal cord compression?
Many causes of spinal cord compression can’t be prevented. You can help prevent symptoms of spinal cord compression caused by gradual wear and tear by keeping the muscles and bones of your back as strong and healthy as possible.
- Get regular exercise. Exercise makes the muscles that support your back stronger and helps keep your spine flexible.
- Maintain good posture and learn how to safely lift heavy objects. Other good body mechanics include sleeping on a firm mattress and sitting in a chair that supports the natural curves of your back.
- Maintain a healthy weight. Excess weight puts more stress on your back. It can contribute to developing symptoms of spinal compression.
- Eat a well-balanced diet.
- Don't smoke.
How is spinal cord compression managed?
The best way to manage spinal cord compression is to learn as much as you can about your condition, work closely with your healthcare providers and caregivers, and take an active role in your treatment.
Keep your back as healthy as possible. Stay at a healthy weight. Practice good body mechanics. Get regular exercise.
Simple home remedies like an ice bag, heating pad, massage, or a long hot shower can help reduce pain.
The nutritional supplements glucosamine and chondroitin have been recommended as nutritional supplements for people with osteoarthritis. But recent studies have been disappointing. Ask your healthcare provider if they recommend any supplements for you. And always discuss any alternative treatments or medicines you’d like to try.
When should I call my healthcare provider?
Spinal cord compression or cauda equina syndrome (compression of nerve bundle in lower spine) is a medical emergency. Call your healthcare provider or go to the emergency room if you have:
- Sudden loss of bowel or bladder control
- Severe or increasing numbness between your legs, inner thighs, or back of your legs
- Severe pain and weakness that spreads into one or both legs, making it hard to walk or get out of a chair
Key points about spinal cord compression
- Spinal cord compression is caused by a condition that puts pressure on your spinal cord.
- Symptoms, such as pain, numbness, or weakness in the arms, hands, legs, or feet, can come on gradually or more suddenly, depending on the cause.
- Spinal cord compression can often be helped with medicines, physical therapy, or other treatments. Except in emergencies, surgery is usually a last resort.
- Keep your back healthy by living a healthy lifestyle. This includes staying at a healthy weight, eating a well-balanced diet, not smoking, and getting regular physical activity.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.
Back and Neck Pain
What is back and neck pain?
Back pain can range from a mild, dull, annoying ache to persistent, severe, disabling pain. Pain in your back can limit your ability to move. It can interfere with normal functioning and quality of life. Always talk with your healthcare provider if you have persistent pain.
Neck pain occurs in the area of the cervical vertebrae in your neck. Because of its location and range of motion, your neck is often left unprotected and at risk for injury.
Pain in your back or neck area can come on suddenly and intensely. Chronic pain lasts for weeks, months, or even years. The pain can be constant or come and go.
What causes back and neck pain?
Even with today's technology, the exact cause of back and neck pain is hard to find. In most cases, back and neck pain may have many different causes. They include:
- Overuse, strenuous activity, or incorrect use, such as repetitive twisting or heavy lifting
- Trauma, injury, or fractures
- Breakdown of vertebrae, often caused by stresses on the muscles and ligaments that support your spine, or the effects of aging
- Infection
- Abnormal growth, such as a tumor or bone spur
- Obesity, which puts extra weight on your spine and pressure on your disks
- Poor muscle tone or muscle weakness in the back and belly (abdomen)
- Muscle tension or spasm
- Sprain or strain
- Ligament or muscle tears
- Joint problems, such as arthritis
- Smoking
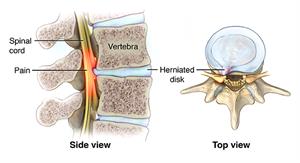
- Slipped disk (protruding or herniated disk) and pinched nerve
- Osteoporosis and compression fractures
- Problems of your vertebrae and bones that you were born with (congenital)
- Abdominal problems, such as an aortic aneurysm
What are the symptoms of back and neck pain?
Symptoms linked to back pain may include:
- Dull, burning, or sharp pain in your back. The pain can be limited to a single spot or cover a large area.
- Leg numbness or tingling above or below your knee
- Stiffness or aching that occurs anywhere along your spine from your neck to your tailbone
- Sharp, shooting pain that spreads from your low back to your buttocks, down the back of your thigh, and into your calf and toes
- Consistent ache in the middle or lower part of your back, especially after standing or sitting for a long period
Loss of bladder and bowel control with weakness in both legs are symptoms of a serious condition that needs medical attention right away.
Symptoms linked to neck pain can be:
- Arm numbness or tingling
- Headaches
- Shoulder pain
- Sharp shooting pain or a dull ache in your neck
Pain that occurs suddenly in your back or neck from an injury is acute pain. Acute pain comes on quickly and may leave sooner than chronic back or neck pain. This type of pain should not last more than 6 weeks.
Pain that may come on quickly or slowly and lingers for 3 months or more is chronic pain. Chronic pain is less common than acute pain.
How are back and neck pain diagnosed?
Your healthcare provider will ask about your health history and do a physical exam. They may also do X-rays of the affected areas, as well as an MRI. This allows a more complete view. The MRI also makes pictures of soft tissues such as ligaments, tendons, and blood vessels. The MRI can help spot infection, tumor, inflammation, or pressure on your nerve. Sometimes a blood test may help diagnose arthritis, a condition that can cause back and neck pain.
How are back and neck pain treated?
In many cases, acute back or neck pain may simply improve with some rest. Over-the-counter medicines, such as acetaminophen or ibuprofen, may also help with the discomfort. Try to move gently during this period, so that you won't become stiff and lose mobility.
If you have chronic pain of your back and neck, try several remedies before considering surgery. These include:
- Hot or cold packs as advised by your healthcare provider
- Certain exercises to strengthen back and belly muscles and ease pain, such as stretching and flexing. Your healthcare provider can show you these exercises. Physical therapy can also help you find the correct exercises.
- Aerobic exercise may help with your overall fitness and strength.
- Certain anti-inflammatory medicines or muscle relaxants may be used, as advised by your provider.
- Sometimes your provider may suggest a brace or corset for extra support.
- Shots (injections) for pain relief in the area
- Nerve block. This eases pain signals from the affected nerve.
- Acupuncture
- Osteopathic manipulation
How are back and neck pain managed?
Acute back pain usually gets better without special treatment. Using acetaminophen or ibuprofen as directed will decrease pain and help you rest. Surgery and special exercises are generally not used with acute pain.
For severe, disabling, or chronic back and neck pain, rehabilitation programs can be designed to meet your needs. The type of program will depend on the cause and the type and severity of your pain, injury, or disease. Your active involvement is key to the success of rehab programs.
The goal of back and neck rehab is to help you manage disabling pain. It's also important to return you to your highest level of functioning and independence and improve your quality of life. The focus of rehab is on easing pain, improving movement. It also focuses on limiting any additional damage and increasing your functional ability.
To help reach these goals, back and neck rehab programs may include:
- Exercise programs to improve range of motion, increase muscle strength, improve flexibility and mobility, and increase endurance
- Help with assistive devices that keep you independent
- Education and counseling
- Pain management methods
- Help to quit smoking
- Gait (walking) and movement retraining
- Stress management
- Nutritional counseling
- Ergonomic assessments and work-related injury prevention programs
- Job counseling
What are possible complications of neck and back pain?
Complications of back and neck pain may include:
- Loss of productivity. Back pain is the most common reason for disability in working adults.
- Nerve damage. If your back pain is from a herniated disk, pressure on the spinal nerves may cause a variety of problems, such as weakness, numbness, or severe shooting pain that travels from the back to the leg.
- Depression. Back or neck pain can disrupt all aspects of life. This includes work, physical exercise, social activities, and sleep. The anxiety and stress caused by the change in movement and pain can lead to depression.
- Weight gain. Loss of movement and inability to exercise can lead to weight gain and the loss of muscle strength.
It is a good idea to see a healthcare provider if you have numbness or tingling, or if your pain is severe and does not get better with medicine and rest. If you have trouble urinating, weakness, pain, or numbness in your legs, fever, or unintentional weight loss, call your healthcare provider right away.
Can I prevent neck and back pain?
The following may help to prevent back and neck pain:
- Practice correct lifting methods. Don't lift heavy items. When you do lift something, bend your legs, keep your back straight, and then slowly lift your body and the object.
- Wear a seat belt in motor vehicles in case of a collision.
- Use telephones, computers, and other equipment correctly.
- Maintain correct posture while sitting, standing, and sleeping.
- Exercise regularly. Learn back-strengthening exercises to keep your back and belly muscles strong. Warm up with stretching exercises before doing exercises.
- Do exercises that improve your balance.
- Don't smoke.
- Stay at a healthy weight.
- Reduce emotional stress that may cause muscle tension.
- Get enough vitamin D and calcium in your diet.
When should I call my healthcare provider?
See your healthcare provider if you have:
- Loss of bladder or bowel control with weakness in either leg. These symptoms need attention right away.
- Severe back or neck pain that does not decrease with medicine and rest
- Pain after an injury or a fall
- Weakness, numbness, or tingling in your legs or arms
- Fever of 100.4°F (38°C) or higher, or as advised by your healthcare provider
- Unintentional weight loss
Key points about back and neck pain
- Back and neck problems range from minor aches to severe, disabling pain.
- Often, the reason for your pain can't be found.
- See a healthcare provider if you have numbness or tingling, severe pain that does not improve with medicine and rest, trouble urinating, weakness, pain, or numbness in your legs, fever, unintentional weight loss, or pain after a fall.
- Often, back and neck pain will improve over time. See your healthcare provider if your pain is not decreasing.
- Use prevention strategies to keep yourself healthy and injury-free.
- For severe, disabling, or chronic back pain, consider an individualized rehabilitation program.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new directions your provider gives you.
- Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.
Epidural Corticosteroid Injections
What is an epidural corticosteroid injection?
In the simplest of terms, an epidural corticosteroid (steroid) injection is a way to deliver medicine quickly into the body with a syringe. It is done to help relieve pain.
The medicine is injected into the epidural area. This is a fat-filled area that covers the spinal cord to protect it and the surrounding nerves from damage.
Sometimes pain relief is short-term. Other times the benefits continue for some time. This procedure is usually part of a treatment plan that may also include physical therapy, exercise, lifestyle changes, and oral anti-inflammatory medicines.
Why might I need an epidural steroid injection?
If you have intense, difficult-to-treat pain in your legs or arms from inflamed spinal nerves, then an epidural steroid injection might give you quick relief. Often, nerve passages from the spine to your arms or legs become narrowed, causing this pain. This narrowing can cause inflammation of the spinal nerves.
A number of conditions may add to this narrowing, including:
- Herniated disks
- "Slipped" vertebrae
- Joint cysts
- Bone spurs
- Thickening ligaments in the spine because of spinal arthritis
Injected steroids reduce inflammation and open up these passages to provide pain relief.
What are the risks of an epidural steroid injection?
An epidural steroid injection generally causes no problems. If you do have side effects, they may include:
- "Steroid flush," or flushing of the face and chest, with warmth and an increase in temperature for several days
- Increased blood sugar
- Pain at the injection site
- Skin discoloration at the injection site
- Sleeping problems
- Anxiety and irritability
- Menstrual changes
- Leg swelling
- In rare instances, pain that actually increases for several days after the procedure
Serious complications are rare but can include:
- Allergic reaction
- Bleeding
- Nerve damage
- Infection
- Paralysis
How do I get ready for an epidural steroid injection?
You will be asked to read and sign a document called an informed consent form. Be sure to read the document carefully and ask questions before you sign.
Tips for preparation include the following:
- An epidural steroid injection is generally an outpatient procedure. You may be asked to change into a surgical gown to make the injection process easier.
- You may want to ask for a mild sedative, but most people receive just local anesthetic.
- If you have diabetes, an allergy to contrast dye, or certain other medical conditions, you'll want to discuss any concerns with your healthcare provider before getting the procedure.
Based on your medical condition, your healthcare provider may request other specific steps.
What happens during an epidural steroid injection procedure?
An epidural steroid injection is a simple procedure:
- Your healthcare provider will use an X-ray machine showing moving images on a screen to guide the needle as the healthcare provider makes the injection and ensures that the needle is in the correct location.
- Contrast dye is injected at the site to make sure that the medicine will be sent to the exact place it needs to go.
- The healthcare provider will inject the steroid medicine itself, often along with a local anesthetic to help with pain relief.
What happens after an epidural corticosteroid injection procedure?
Once the procedure is done, you can return home. Usually, you'll be able to return to normal activities on the next day. The steroids usually start working within 1 to 3 days. In some cases, you might need up to a week to feel the benefits.
Many people get several months of improvement of pain and function from the injections. If the injection is effective, it can be repeated. If you have any side effects, be sure to contact your healthcare provider.
If you don't have pain relief, talk with your healthcare provider.
This may be a sign that the pain is coming from someplace other than the spinal nerves.
After the procedure, seek urgent medical care right away if you have:
- Severe headache with nausea and vomiting
- Fever
- Loss of bowel or bladder control
- New onset of numbness or tingling
Next steps
Before you agree to the test or the procedure, make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how you will get the results
- Who to call after the test or procedure if you have questions or problems
- How much you will have to pay for the test or procedure