Pancreatic Cancer
Saint Luke’s Cancer Specialists provide early detection, expert diagnosis, personalized treatment options, and survivorship support to every patient.
We offer comprehensive treatment options. If surgery is needed, the Saint Luke’s Liver Biliary & Pancreatic Center provides expert surgical care for pancreatic cancer patients.
When facing a pancreatic cancer diagnosis, you want an experienced team on your side. Saint Luke’s is the only cancer program in Kansas City to be nationally recognized as an NPF Pancreatic Cancer Center by the National Pancreas Foundation. This designation is reserved for programs that specialize in the multidisciplinary treatment of pancreatic cancer. Our care team includes leading experts in medical and radiation oncology, surgery, and precision oncology. They work together to customize a treatment plan tailored to your unique needs.
What Is Pancreatic Cancer?
What Is Pancreatic Cancer?
Cancer starts when cells in the body change and grow out of control. These cells can form lumps called tumors. Cancer that starts in the cells of the pancreas is called pancreatic cancer.
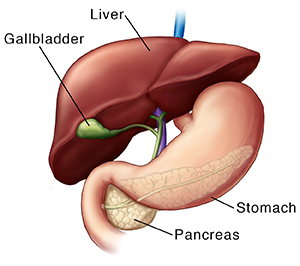
Understanding the pancreas
The pancreas is a gland, an organ that makes substances the body needs. It's located in the left side of the belly (abdomen), behind the stomach and in front of the spine.
The pancreas has two main jobs:
- It makes pancreatic enzymes . These enzyme juices help digest food. They go into the small intestine to help break down food.
- It makes hormones . These include insulin and glucagon. They help control the amount of sugar (glucose) in the blood.
When pancreatic cancer forms
Pancreatic cancer forms when cells in the pancreas change (mutate) and grow out of control. This can change the way the pancreas works. Pancreatic cancer can spread into nearby organs, like the intestines, liver, and gallbladder. It can also spread to other parts of the body. This spread is called metastasis. The more cancer spreads, the harder it is to treat.
Treatment choices for pancreatic cancer
You and your healthcare provider will talk about treatment and make a plan that's best for you. Your treatment choices may include:
-
Surgery. This removes the cancer in the pancreas. Sometimes nearby tissues and organs are also removed.
-
Radiation therapy. This aims high-energy X-rays at the tumor to kill cancer cells.
-
Chemotherapy. This uses strong medicines to kill fast-growing cells like cancer cells. Chemotherapy and radiation therapy can also be given together. This is called chemoradiation.
- Immunotherapy or biologic therapy. This uses medicines that boost the body's natural immune system to better fight the cancer.
- Targeted therapy. This uses medicines that focus on specific changes found only or mostly on the cancer cells, such as genetic changes or proteins. These medicines then kill the cancer cells. But it limits damage to normal cells.
Diagnosis
Pancreatic Cancer: Diagnosis
If your healthcare provider thinks you might have pancreatic cancer, you’ll need certain exams and tests to be sure. The process starts with your healthcare provider asking you questions. You'll be asked about your health history, symptoms, risk factors, and your family history of disease. A physical exam will be done, focusing on your belly.
Based on the findings, your healthcare provider will decide what other tests are needed.
What tests might I need?
You may need one or more of these tests:
Blood tests
Imaging and endoscopy tests
Pancreatic biopsy
Blood tests
You may have blood tests to look for signs of pancreatic cancer.
Liver function tests (LFTs)
These tests look for certain chemicals in your blood to get an idea of how well your liver is working. They can sometimes help tell if a bile duct is blocked. This might be caused by a pancreatic tumor. Still, LFTs can't tell for sure if you have pancreatic cancer because there are other causes of blocked bile ducts. But if the results of these tests are abnormal, your healthcare provider may do other tests to check for cancer.
CA19-9 marker
CA19-9 is a tumor marker. It’s a substance that can sometimes be found in high levels in your blood if you have cancer. This test by itself can't diagnose pancreatic cancer. That's because not everyone who has pancreatic cancer has a high CA19-9 level. Plus, sometimes people have a high CA19-9 level without having pancreatic cancer. But if this test is abnormal, your healthcare provider might do other tests to look for pancreatic cancer.
Imaging and endoscopy tests
Your healthcare provider may use imaging and endoscopy tests to look for pancreatic cancer. Imaging tests use things like X-rays and sound waves to take pictures of the inside of your body. For endoscopy tests, a thin tube (called an endoscope) is put into your body. A camera at the end of the tube lets your healthcare provider look at your organs and other tissues.
Ultrasound
An ultrasound uses sound waves to look for changes in your pancreas and bile ducts. The sound waves bounce off body parts and send back a series of signals. A computer turns these into images of your insides. This might be the first test you have because it’s easy and doesn’t use radiation. During an ultrasound, the sound waves come from a wand-like device that’s moved over the skin on your belly (abdomen) and aimed at your pancreas.
For an endoscopic ultrasound (EUS), the images of the pancreas are taken from inside your body. This makes a better picture. Medicines are used to make you sleep for this test. Then a thin, lighted tube (called an endoscope) is put down your throat, through your stomach, and into the first part of your small intestine. At the tip of the endoscope is a tiny ultrasound device. It bounces waves into nearby tissues, including the pancreas, to make images on a computer screen. During the test, if your healthcare provider sees anything of concern, a small, hollow needle may be passed through the endoscope to take out a small piece (sample) of tissue. This is called a biopsy.
CT scan
A CT scan uses X-rays taken from many angles. It creates very detailed cross-section pictures of your pancreas and nearby tissues. CT scans can often show pancreatic tumors and blocked bile ducts.
Sometimes a special type of CT scan called a pancreatic protocol CT is used. For this scan, a contrast dye is put into your blood to make images clearer. Over a certain time, pictures are taken of the pancreas before the contrast is injected and multiple times as the dye moves through it. This can help your healthcare team see if surgery to take out the pancreas might be an option.
PET (positron emission tomography) scan
For this test, a radioactive sugar is put into your blood through a vein in your arm or hand. Over time, the radioactive sugar collects in very active cells, like cancer cells. A special camera is then used to make pictures that show where the radioactive sugar collects. The picture from this test is not as detailed as a CT scan. It isn’t used alone to diagnose pancreatic cancer. But it can still sometimes be helpful. A PET scan may be done in combination with a CT scan (PET/CT scan).
MRI (magnetic resonance imaging)
This test uses magnets and radio waves to create detailed images of your pancreas and nearby organs. While MRIs can show more detail than other imaging tests, they aren’t used as often as CT scans when looking for pancreatic cancer.
ERCP (endoscopic retrograde cholangiopancreatography)
This test is a type of X-ray used to look at the bile ducts and the pancreatic duct. Medicines are used to make you sleep. Then a long, thin tube (endoscope) is put down your throat, through your stomach, and into your small intestine. A smaller tube (catheter) is slid through the scope into the common bile duct. Dye is then injected through the catheter. It goes into your bile and pancreatic ducts. The dye shows up on X-rays. This can show ducts that might be blocked or narrowed by a tumor. If your healthcare provider sees anything that doesn't look normal, a tissue sample (biopsy) might be taken out and checked for cancer.
MRCP (magnetic resonance cholangiopancreatography)
This test is a lot like an ERCP, but it uses an MRI instead of an endoscope. MRCP can show both the bile ducts and the pancreatic duct without the need to put a scope in them. But if your healthcare provider sees something that doesn't look normal, a biopsy can't be done during this test.
PTC (percutaneous transhepatic cholangiography)
This is another type of X-ray of the bile duct. A thin needle is put through the skin on the right side of your belly and into your liver. A dye is then injected through the needle. The dye highlights blockages in bile ducts, which can then be seen on an X-ray. If a blocked bile duct is seen, your healthcare provider may take a biopsy and check it for cancer. This test is mostly done if an ERCP can't be done.
Pancreatic biopsy
If an imaging test shows something in your pancreas that looks like it might be cancer, your healthcare provider may take out small pieces (called samples) of the changed tissue. This is called a biopsy.
A biopsy is usually the only way to be sure that a person has pancreatic cancer. A healthcare provider who specializes in looking at cells, called a pathologist, looks at the samples under a microscope. Tests are done to see if they contain cancer. There are different types of biopsies. The type of biospy, in part, depends on where the cancer may be located and the plan for treatment. Several samples should be taken for diagnosis and to perform tests to see if the cancer cells have specific genetic changes (mutations).
Percutaneous (through the skin) needle biopsy
For this test, a thin, hollow needle is put through your skin and into the pancreatic tumor to get a sample of it. A CT scan or ultrasound of the pancreas is usually used to help your healthcare provider guide the needle into the tumor.
Endoscopic biopsy
During procedures such as endoscopic ultrasound or ERCP, your healthcare provider may pass long, thin tools down the scope to take samples of areas that don't look normal. This might be done with a thin, hollow needle or a tiny brush.
Laparoscopic biopsy
For this test, your surgeon makes a small cut (incision) in your skin over your belly. A thin tube with a light and a tiny video camera on the end is put into this cut. This lets your healthcare provider see your pancreas and nearby areas. Other small cuts may be made to put in other tools to remove cells for testing. This procedure isn't done as often as in the past.
Getting your test results
When your healthcare provider has the results of your tests, they'll contact you. Ask how you can expect to find out your biopsy results. Will it be a phone call, or do you need to make an appointment?
Your healthcare provider will talk with you about other tests you may need if pancreatic cancer is found. Make sure you understand the results and what your next steps should be.
Treatment Choices
Pancreatic Cancer: Treatment Choices
Various types of treatment can be used for pancreatic cancer. Which may work best for you? It depends on a number of factors. These include the size, location, and stage of your cancer. Factors also include your age, overall health, and what side effects you’ll find acceptable.
Learning about your treatment choices
You may have questions and concerns about your treatment choices. You may also want to know how you’ll feel and function after treatment, and if you’ll have to change your normal activities.
Your healthcare provider is the best person to answer your questions. They can tell you what your treatment choices are, how successful they’re expected to be, and what the risks and side effects are. Your healthcare provider may suggest a specific treatment. Or they may offer more than one, and ask you to decide which you’d like to use. It can be hard to make this decision. It's important to take the time you need to make the best decision.
Deciding on the best plan may take some time. Talk with your healthcare provider about how much time you can take to explore your choices. You may want to get another opinion before deciding on your treatment plan. You also may want to include your family and friends in this process.
Understanding the goals of treatment for pancreatic cancer
For some pancreatic cancers, the goal of treatment is to cure the cancer. If cure isn’t possible, treatment may be used to shrink the cancer or keep it under control for as long as possible. Treatment can also improve your quality of life by helping to control the symptoms of the disease. The goals of treatment can be one or more of these things:
-
Remove or destroy the cancer in your pancreas
-
Remove or destroy tumors in other parts of your body
-
Stop or slow the growth or spread of pancreatic cancer cells
-
Prevent or delay the cancer from coming back
-
Ease symptoms caused by the cancer. These can include pain or pressure on your organs.
Types of treatment for pancreatic cancer
Many types of treatment can be used for pancreatic cancer. Different combinations of treatment may be used. These depend on a number of factors, such as:
-
The size of the cancer and where it is
-
The stage (extent) of the cancer
-
Your age and overall health
-
Your personal concerns and preferences
Surgery
This is often the preferred treatment for early stage pancreatic cancer if it can be done. This is because it may cure the cancer. But in most cases, pancreatic cancer has spread too far to be removed completely. If the cancer can’t be removed, your healthcare provider might still suggest a less extensive surgery to ease symptoms.
Radiation therapy
This treatment is often used with chemotherapy (chemo), either before or after surgery. Radiation and chemo before surgery can help shrink a tumor and make it easier to take out. After surgery, radiation and chemo can be used to try to kill any cancer cells that are left. Radiation may also be used as part of the main treatment in people who can't have surgery. Or it may be used to help ease symptoms in people with advanced cancer.
Chemotherapy
Chemo uses strong medicines to kill cancer cells. For pancreatic cancer, chemo may be used before or after surgery (often with radiation). Or it may be the main treatment for people who can't have surgery.
Targeted therapy
These medicines target specific parts of cancer cells that help the cancer grow and spread. Targeted therapy medicines work differently from standard chemo medicines, and they have different side effects. They may be used along with chemo in some cases.
Immunotherapy
These medicines help your immune system find and kill cancer cells. These medicines may be used if pancreatic cancer comes back, can't be treated with surgery, or has spread.
Supportive care
Your healthcare provider may suggest treatments that help ease your symptoms, but don’t treat the cancer. For instance, you may need treatment to help with nausea or pain. These can be used along with other treatments. Your provider may suggest you get only supportive care if they believe that the available cancer treatments are more likely to do you more harm than good.
Clinical trials for new treatments
Researchers are always looking for new and better ways to treat pancreatic cancer. These new methods are tested in clinical trials, a type of research study. Talk with your healthcare provider to find out if there are any clinical trials you should consider.
Talking with your healthcare provider
At first, thinking about treatment choices may seem overwhelming. Talk with your healthcare team and loved ones. Make a list of questions. Consider the benefits and possible side effects of each choice. Talk about your concerns with your healthcare provider before making a decision.
Pancreatic Cancer Statistics
Pancreatic Cancer: Statistics
What are statistics?
Some people use numbers called statistics to figure out their chances of getting cancer. Or they use them to try to figure out their chances of dying from cancer. Because no 2 people are alike, statistics can’t be used to predict what will happen to 1 person. The statistics below describe large groups of people. They do not take into account a person's own risk factors, such as family history, behaviors, or cancer screenings. If you have questions, talk with your healthcare provider.
What are the statistics for pancreatic cancer?
Here are some statistics about pancreatic cancer:
About 55,440 new cases of this cancer will be diagnosed in the United States in 2018.
About 44,330 people will die of pancreatic cancer in 2018.
The average person's risk of getting this cancer in their lifetime is about 1 in 65 for women and 1 in 63 for men. Your chance of getting this cancer may be higher or lower. This depends on your risk factors.
Source: American Cancer Society
Clinical Trials
A Phase III Study of BBI-608 plus nab-Paclitaxel with Gemcitabine in Adult Patients with Metastatic Pancreatic Adenocarcinoma
Randomized Phase II Study of Perioperative mFOLFIRINOX Versus Gemcitabine/Nab-Paclitaxel as Therapy for Resectable Pancreatic Adenocarcinoma
A Phase IB/II Randomized Study of Modified FOLFIRINOX + Pegylated Recombinant Human Hyaluronidase (PEGPH20) Versus Modified FOLFIRINOX Alone in Patients with Good Performance Status Metastatic Pancreatic Adenocarcinoma
A Phase II-R and a Phase III Trial Evaluating Both Erlotinib (Ph II-R) and Chemoradiation (Ph III) as Adjuvant Treatment for Patients with Resected Head of Pancreas Adenocarcinoma
A Phase II Study of MLN0128 (TAK-228) in Rapalog-Resistant Advanced Pancreatic Neuroendocrine Tumors (PNET)
Preoperative Extended Chemotherapy vs. Chemotherapy Plus Hypofractionated Radiation Therapy for Borderline Resectable Adenocarcinoma of the Head of the Pancreas
Providers

Norin Ansari, MD, MPH

Juliet Gyamfua Appiah, MD
Sreekanth Donepudi, MD

Jameson Forster, MD
Sashidhar Manthravadi, MD

Megan E McNally, MD

Marc T Roth, MD

Kathryn W Shaw, MD
Eston James Schwartz, MD

Addison R Tolentino, MD
Matthew B Wilkinson, MD, PhD

